60 Hospital Event Form
Medical Expenditure Panel Survey - Household and Medical Provider Components
Attachment 60 -- Hospital Event Form
OMB: 0935-0118
MEDICAL EXPENDITURE PANEL SURVEY
MEDICAL PROVIDER COMPONENT
EVENT FORM
FOR
HOSPITAL PROVIDERS
Combined MEDICAL and billing RECORDS
REFERENCE YEAR 2022
Specifications for RCD
Version # |
Generation of changes |
date to AHRQ |
1.0 |
Updates made for 2022 data collection – highlights in yellow |
12/20/22 |
|
|
|
|
|
|
|
|
|
|
|
|
programming note for HEADER:
IN THE UPPER LEFT, ADD a subheader that reads. REFERENCE is “left label”. put the prelogic in the sections instead of forms.
“Medical records” for question a1 through mr ending
“PATIENT ACCOUNTS” for EVTCONFIRM/intro through pa ending.
ALSO IN THE TOP LEFT OF THE EVENT FORM, add a subheader that reads:
PATIENT NAME
“on mm-dd-yyyy”, to fill with DATE REPORTED IN OUTPAT_DATE (IF OP PATH) OR “from MM-DD-YYYY through MM-DD-YYYY” TO FILL WITH DATES REPORTED IN INPATBEG_DAT and INPATEND_DAT (IF ip PATH).
EVENT FORM #, TO FILL WITH EVENT FORM ID
PROGRAMMERS: This document details the specifications for the Hospital Medical Event Form. We have provided specifications for the overall screen design as well as question by question specifications.
Overall functionality requirements we would like for the system controlling the event forms are as follows:
Show an “overall” progress indicator on the screen.
Set up FUNCTION KEYS for each of the following commands:
Don’t Know
Refused
The function keys would be available for any question unless specified otherwise in the question by question specifications.
The “Help” menu at the top left would list the DK and REF buttons for the DCS/Abstractor.
NOTE: 2018 Update: The response option of “Retrievable” was removed from all Event Forms.
To assist the DCS/abstractors if they need to jump around a form, among forms, and among patients for a given provider:
Within an event form, in addition to post-logic, include pre-logic to the area we are skipping to, so the interviewer wouldn’t be able to access a group of questions without answering the gateway question. For example, the “Capitated Basis” section should not allow entry unless the question in “Reimbursement Type” (C3) = 2.
Incorporate edit trails (e.g., if need to go back and revise answer).
Include in the screen header some sort of progress status on how many patients for a given provider have been completed out of the total (e.g., Done with 2 of 3 patients).
Allow the DCS/abstractors to see a list of the event forms completed for a given patient (with event dates) in case they need to go back to revise some information in one of the forms.
Once the DCS/abstractors finish with one patient they are taken back to a summary screen listing all patients for that provider, so they can click on the next patient.
Question By Question Specifications
The QxQ specifications have been broken out throughout the rest of this document by section and include the screen layout, programmer notes, and edit specifications from Westat.
NOTE:
Westat EDIT SPECS:
Westat editors wrote BLUE SHEETS to the TRC (telephone research center) for data items that needed collection, clarification, or correction. The TRC is our contact with the respondent in the provider’s office.
Westat editors wrote YELLOW SHEETS for problematic items that needed managerial review.
NOTE:
The following are a list of CRITICAL ITEMS and ADDITIONAL DATA RETRIEVAL ITEMS in the event form, which were pulled from (1) the CHEAT SHEET provided by AHRQ with the edit specs (cheat sheet rev2 DRG after 10-1-07.doc found in \\rtints27\meps\00_Admin\04_Documents\Materials From AHRQ and Westat\11_14_2008\Docs_Received_Electronically\MPC_Edit_Specx.zip) and (2) the following memo \\RTINTS27\MEPS\01_BASE_YEAR\11_DATA_COLLECTION\00_DCT_COMMON\REQUESTS_FOR_CLIENT\FROM CLIENT\CRITICAL DATA ITEMS MEMO 01051997.PDF
CRITICAL ITEMS
EVENT DATE - Inpatient/LTC – admit/discharge dates
At least month and year must be recorded.
EVENT DATE - Outpatient/ER/Other – visit date
At least month and year must be recorded.
SERVICES/CHARGES – OUTPATIENT/ER/OTHER
At least one procedure code or description must be recorded.
SERVICES/CHARGES – INPATIENT/LTC
A8 must have a DRG, OR, A9 must be no, OR, if A9 is yes, there must be at least one procedure code or description in A10.
REIMBURSEMENT
Fee for service or capitated must be circled.
SOURCE OF PAYMENTS
The amount paid by each source must be recorded, OR the total payments and the contributing source must be recorded. This includes OTPAYMOS and OTPAYMOSTXT.
OTHER GLOBAL FEE DATES - A5_EVNTBEG_DATE
omb Statement
DCS: IN GENERAL, PRESS <F6> FOR DON’T KNOW and <F7> FOR REFUSAL. AT ANY POINT, PRESS <F2> FOR SHORTCUT TO ALL DK/RF RESPONSES. USE UP/DOWN ARROWS OR PAGE UP/DOWN TO MOVE THROUGH RESPONSES. PRESS END BUTTON TO JUMP TO THE LAST OPEN QUESTION.
READ THIS ALOUD ONLY IF REQUESTED BY RESPONDENT.
OMB Statement:
Public reporting burden for this collection of information is estimated to average 3 minutes per response, the estimated time required to complete the survey. An agency may not conduct or sponsor, and a person is not required to respond to, a collection of information unless it displays a currently valid OMB control number. Send comments regarding this burden estimate or any other aspect of this collection of information, including suggestions for reducing this burden, to: AHRQ Reports Clearance Officer Attention: PRA, Paperwork Reduction Project (0935-0118) AHRQ, 5600 Fishers Lane, Rockville, MD 20857.
OMB No. [#]; Exp. Date [DATE]
CONTINUE
SECTION 1 – MEDICAL RECORDS – Location of Services
[Page 1 – MEDICAL RECORDS - Location of Services (1 of 1)]
ScreeN LAYOUT
|
|
A1. The (first/next) time (PATIENT NAME) received services during calendar year 2022, were the services received: CODE ONLY ONE
|
As an Inpatient 1 MREVTYPE In a Hospital Outpatient Department 2 In a Hospital Emergency Room 3 In a Long Term Care unit such as skilled nursing facility …………5 Somewhere else? ……………………………………………………4
(IF SOMEWHERE ELSE: Where was that?) MREVTYOS 6. Ambulance 9. Hospital Free Standing Clinic/ Hospital Satellite Clinic 5. Independent Facility 15. Independent Pathology Clinic. Laboratory, Clinical Lab 14. Independent Radiology Clinic, Imaging CTR, X-Ray 13. Observation, Ambulatory Surgery Center 2. SurgiCenter 16. Telehealth 17. Drive-through 91. Other
IF SOMEWHERE ELSE:Specify other location MREVTYOSTXT |
|
|
PROGRAMMER NOTES
2017 UPDATE: Remove “IF INPATIENT” dropdown from A1.
[IF MREVTYPE=1 or 5 GO TO A2a,
IF MREVTYPE =2 or 3 or 4 GO TO A2c]
(first/next): If first event form for patient fill: "first" ELSE fill: "next".
(PATIENT NAME) should fill with patient’s first name and patient’s last name from Housing Component data file.
MREVTYOS The “somewhere else” option should be set up so a response can be selected from a list, or entered in as text. The options should include: Observation, Ambulatory Surgery Center; SurgiCenter; Independent Radiology Clinic, Imaging CTR, X-Ray; Independent Pathology Clinic. Laboratory, Clinical Lab; Independent Facility; Ambulance; Hospital Free Standing Clinic/ Hospital Satellite Clinic; Telehealth; Drive-through; Other. See decision log (below) for instructions on behind the scenes recoding.
MREVTYOSTXT will hold the 30-character text box response for the free-form text entry required when MREVTYPE=4 and MREVTYOS=91.
DO NOT ALLOW DK/REF TO MREVTYPE (event form requires correct coding of A1 for correct path through instrument). However, MREVTYOS and MREVTYOS2 should allow DK/REF.
EDIT SPECS FROM WESTAT
-
DATA ITEM
SPECIFICATIONS
ACTION, if specification not met
QA1 - Where event took place
USED FOR
DETERMINING SBDs
1, 2, 3, 4, or 5 must be circled.
Blue Sheet.
Only one response can be chosen.
Blue Sheet.
If 4 (Somewhere Else) is answered, there must be an answer on the SPECIFY line.
If 5 (Long Term Care Unit) is answered, there must be an answer on the SPECIFY LINE.
Blue Sheet, if blank and answer can’t be determined.
If there is a comment explaining what the Specify answer should be, look it up on the Decision log. If it can be accepted, circle it. If it is not on the Decision Log, Yellow Sheet.
Answer on the SPECIFY line needs review.
Check Decision log.
If answer is on the Decision Log, accept.
If the answer is not on Decision Log, Yellow Sheet
Institution cases are edited only by specially-trained editors.
Procedure must be compatible with event type (location of event).
Compare procedure to location of event.
Yellow Sheet, if not compatible.
See Special Procedure Notes, pages 5-22 to 5-23.
For IC procedures, 5 must be circled and Other/Specify answer must be given.
Circle 5 and record INSTITUTION as the Other/Specify location.
Decision Log for QA1
Question - Form Type |
Problem |
Decision / Categorization |
QA1 - Hosp Location of Event |
|
|
Answer is (4) |
Observation |
Code QA1 as 2 (Outpatient) |
or (5) |
Ambulatory Surgery Center |
Code QA1 as 2 (Outpatient) |
And |
SurgiCenter |
Code QA1 as 2 (Outpatient) |
QA5d - Global fee event type |
Independent Radiology Clinic, Imaging CTR, X-Ray |
Code QA1 as 2 (Outpatient) |
|
Independent Pathology Clinic. Laboratory, Clinical Lab |
Code QA1 as 2 (Outpatient) |
|
Independent Facility |
Code QA1 as 2 (Outpatient) |
|
Ambulance |
Yellow Sheet |
|
SNF |
Code QA1 as 1 (Inpatient) |
|
Rehab Center |
Code QA1 as 1 (Inpatient) |
|
Hospital Free Standing Clinic/ Hospital Satellite Clinic |
Code QA1 as 2 (Outpatient) |
|
Long Term Care Unit |
Code QA1 as 5 and keep as
Specify answer |
|
Institution |
Code QA1 as 5 and keep as Specify answer |
|
Comment indicates one of the above answers |
Code following the
directions above; Change answer following the directions above
if the TRC has answered something else. |
SECTION 2 – MEDICAL RECORDS – EVENT date – Inpatient/LTC (admit/discharge dates)
[Page 3 – MEDICAL RECORDS - eVENT date – INPATIENT/LTC (1 of 1)]
ScreeN LAYOUT
A2a.What was the admit date of the inpatient stay?
What was the discharge date of the inpatient stay?
REFERENCE PERIOD – CALENDAR YEAR 2022
ENTER A DATE IN FORMAT MM/DD/YYYY. INCLUDE LEADING 0’S FOR SINGLE DIGIT MONTHS AND DAYS.
|
ADMIT: INPATBEG_DAT
DISCHARGE: INPATEND_DAT
|
A2b. Was (PATIENT NAME) admitted from the emergency room? |
YES=1, NO=2 ADFROMER |
PROGRAMMER NOTES
INPATBEG_DAT – value for month (MM) should be between 1 and 12
INPATBEG_DAT – value for day (DD) should only valid numbers (1-28 for all months; 29-30 for all months except month 2; 31 allowed only for months 1, 3, 5, 7, 8, 10, and 12; value 29 allowed for month 2 only in leap years)
INPATBEG_DAT – value for year (YYYY) should be 2021 or 2022 (Add soft check for 2020 “WARNING - You have entered a year other than study year. Please review and correct if needed, or suppress and continue.”) (Add hard check for years other than 2021 or 2022 “YEAR MUST BE 2022, PLEASE CORRECT”)
INPATEND_DAT – value for month (MM) should be between 1 and 12
INPATEND_DAT – value for day (DD) should only valid numbers (1-28 for all months; 29-30 for all months except month 2; 31 allowed only for months 1, 3, 5, 7, 8, 10, and 12; value 29 allowed for month 2 only in leap years)
INPATEND_DAT – value for year (YYYY) should be 2022 or 2023 (Add soft check for 2023 “WARNING - You have entered a year other than study year. Please review and correct if needed, or suppress and continue.”) (Add hard check for years other than 2022 or 2023 “YEAR MUST BE 2022, PLEASE CORRECT”)
DISPLAY DCS INSTRUCTION ON A2a INPATEND_DAT: CODE AS “9/9/9999” IF NOT YET DISCHARGED.”
(PATIENT NAME) should fill with patient’s first name and patient’s last name from Housing Component data file.
IF A2a INPATEND_DAT = DK/REF: GO to A2b.
A2b: DK/REF NOT ALLOWED AT THIS QUESTION
A2b go to A3.
EDIT SPECS FROM WESTAT
QA2a INPATIENT (OR IC OR LTC) DOS Follow Skip Pattern
-
DATA ITEM
SPECIFICATIONS
ACTION, if specification not met
QA2a - Dates of Inpatient, or IC, or LTC stay
CRITICAL ITEM
(Month and Year)Admit date and Discharge date must both be present.
Blue Sheet.
Month, day and year are needed.
Blue Sheet if all are blank.
Blue Sheet if month or day is blank.
Blue Sheet if year is blank and can’t be determined.
Fix year, if book is part of a sequence of books in 2022.
Admit date may be in 2021 if Discharge date is in 2022
Discharge date may be in 2023 if Admit date is in 2022.
Blue Sheet if year is wrong, unless it is obvious that it is 2022. If it is in the middle of a sequence of books in chronological order, add 2021 if missing, or change to 2022 if wrong.
Month, and Day are acceptable as DK or RF.
Year is acceptable as DK or RF only after TRC verifies on Blue Sheet.
If month or year is DK or RF, RC code for Pair is 60 – critical item is missing.
Change DK to – 8.
Change RF to – 7.
If year is DK or RF, write a Blue Sheet, asking if at least the year can be determined.
Note: Day is not a critical item.
Duplicate dates need managerial review.
Book dates are same DOS (Date of Service).
Inpatient date range overlaps an OP or ER DOS in another book.
Inpatient date range overlaps a Global Fee date or Repeat Visit date in another book.
Yellow Sheet.
QA2b ADMITTED FROM ER? Follow Skip Pattern
-
DATA ITEM
SPECIFICATIONS
ACTION, if specification not met
QA2b – For HS Event (inpatient stay) – Was the patient admitted from ER?
For IC Event - Is the discharge date given, or is the patient still in the institution?
IC events are transferred from IC to HOSP event books.
1 or 2 must be circled.
If missing, answer can be transferred from Box 4.
Blue Sheet, if Box 4 answer is also missing.
For HS:
If 1 = Admitted from ER, there should be an ER event book.
If 2 = Not Admitted from ER, there should not be an ER event book with a DOS that immediately precedes the HS event DOS.
If answer is 1, Admitted from ER, review other books in the case. Blue Sheet, if there is not an ER event book prior to the inpatient stay.
Answer to QA2b must agree with the answer to Box 4.
Review Box 4.
Yellow Sheet if answers to QA2b and Box 4 are not the same.
FOR IC:
1 = Not yet discharged (Needs managerial review)
2 = Has discharge date
Blue Sheet, if missing and can’t be determined from IC book.
Yellow Sheet, if 1 (Not yet discharged).
Decision Log for QA2b
Question-Form Type QA2b, Box 4, QC2b Linked Books |
Problem |
Decision / Categorization |
|
LINKED BOOKS - ONE BOOK IS NOT IN REFERENCE YEAR |
PER P. WARD AND C. VINCENT 3/3/05 |
|
TRC NOTES THAT CHARGES CANNOT BE BROKEN OUT |
DELETE ER OR OP LINKED BOOK |
BOOK IS NOT IN REFERENCE YEAR, BUT IS LINKED TO BOOK IN REFERENCE YEAR. |
WRITE "DELETED - YEAR ______ LINKED EVENT" ON THE FRONT COVER AND INITIAL COVER |
|
RENUMBER REMAINING BOOKS |
||
CROSS OUT ALL NODES THAT CAME FROM DELETED BOOK |
||
CROSS OUT ANY SBD FORMS THAT ONLY HAD NODES FROM DELETED BOOK |
||
IN LINKED INPATIENT BOOK, QA2B SHOULD SAY "1" YES, ADMITTED FROM ER |
||
IN LINKED INPATIENT BOOK, BOX 4 SHOULD SAY "1" ADMITTED FROM ER |
||
IN LINKED INPATIENT BOOK, QC2b SHOULD SAY "1" EMERGENCY ROOM CHARGE INCLUDED. |
SECTION 3 – MEDICAL RECORDS – EVENT date – outpatient/er/other (visit date)
[Page 4 – MEDICAL RECORDS - eVENT date – Outpatient/ER/other (1 of 1)]
ScreeN LAYOUT
A2c. What was the date of this visit?
REFERENCE PERIOD – CALENDAR YEAR 2022
ENTER A DATE IN FORMAT MM/DD/YYYY. INCLUDE LEADING 0’s FOR SINGLE DIGIT MONTHS AND DAYS. |
A2C_OUTPAT_DATE MONTH/DAY/YEAR
|
PROGRAMMER NOTES
AC2_OUTPAT_DATE – value for month should be between 1 and 12; value for day (DD) should only valid numbers (1-28 for all months; 29-30 for all months except month 2; 31 allowed only for months 1, 3, 5, 7, 8, 10, and 12; value 29 allowed for month 2 only in leap years); value for year should be 2021 or 2022. (Add soft check for 2021 “You have entered a year other than study year. Press Cancel to make a correction or OK to continue.”) (Add hard check for years other than 2021 or 2022 “YEAR MUST BE 2021, PLEASE CORRECT”)
DK/REF – CONTINUE TO A3
EDIT SPECS FROM WESTAT
QA2c ER or OP DATE OF SERVICE Follow Skip Pattern
-
DATA ITEM
SPECIFICATIONS
ACTION, if specification not met
QA2c- Date of OP / ER / Somewhere Else Events
CRITICAL ITEM
(Month and Year)
Month, day and year are needed.
Blue Sheet if all are blank.
Blue Sheet if month or day is blank.
Blue Sheet if year is blank and can’t be determined.
Add year 2022 if year is blank, but book is in the middle of a series of books in 2022.
Year must be 2022
Change year to 2022, if wrong, but book is in the middle of a series of books in 2022.
Blue Sheet if not 2022, and correct date can’t be determined, and book is not linked to a 2022 book.
Delete 2022 or 2022 book linked to 2022 event book. See Link Section, pages 5-24 to 5-25.
Month and Day are acceptable as DK or RF.
Year is acceptable as DK or RF after TRC verifies on Blue Sheet.
If month or year is DK or RF, RC code for Pair is 60 – critical item is missing.
Change DK to – 8.
Change RF to – 7.
Blue Sheet, asking if at least the year can be determined.
Note: Day is not a critical item.
Duplicate dates need managerial review.
More than one book with same DOS.
Book DOS is same as Global Fee or Repeat Visit in this book or another book.
Global Fee or Repeat Visit DOS in this book is same as DOS in another book.
Yellow Sheet.
SECTION 4 – MEDICAL RECORDS – SBD
[Page 5 – MEDICAL RECORDS - SBD (1 of 2)]
ScreeN LAYOUT
PROGRAMMER NOTES
2018 UPDATE: PRELOGIC FOR A3: Create a logic skip around A3 if the VA flag is YES.
(TYPE OF EVENT) should fill with MREVTYPE (A1).
IF MREVTYPE (A1) = 1, fill “inpatient stay”
IF MREVTYPE (A1) = 2, fill “outpatient visit”
IF MREVTYPE (A1) = 3, fill “emergency room visit”
IF MREVTYPE (A1) = 4, fill “visit”
IF MREVTYPE (A1) = 5, fill “institution stay”
(DATE) should fill based on the following logic:
IF MREVTYPE (A1) = 1 or 5, fill “from INPATBEG_DAT through INPATEND_DAT” (A2a).
IF MREVTYPE (A1) = 2, 3, or 4, fill “on A2C_ OUTPAT_DATE” (A2c).
IF A3 ANYSBDS=NO, DK/REF – SKIP TO A4a
IF A3 ANYSBDS=YES, ASK SBD_SOURCE
2019 UPDATE: When no SBDs have yet been added to any events within a contact group, the options available for the SBD_SOURCE item are:
1. ENTER NEW SBD INFO
7. DONE ENTERING SBDs / NO MORE
After SBDs have been entered for any event(s) within a contact group, additional options are displayed at item SBD_SOURCE. In addition to options 1 and 7 (from list above), other options include:
2. SELECT EXISTING SBD
3. UPDATE DATA FOR THIS SBD
4. DELETE THIS SBD ROW
Option 1 allows the entering of information about an SBD new to a contact group.
Option 2 allows an SBD already entered in another event to be selected from an existing list of SBDs entered in other events within the contact group.When an existing SBD is selected, the name and specialty fill, but Service and role do not fill, and must be completed for each new event.The Comments field can also be added for the new event (but is not required to be completed).
Option 3 allows a selected SBD’s GROUP, PREFIX, FIRST, MIDDLE, LAST, NTL_PROVIDER, and SPECIALTY fields to be edited. Edits to these fields will affect all occurrences of a particular SBD within the contact group.
Option 4 deletes a selected SBD and associated information from the current event, but not from the entire contact group.
Option 7 exits the SBD subroutine.
SECTION 5 – MEDICAL RECORDS – SBD Subroutine
[Page 6 – MEDICAL RECORDS - SBD (2 of 2)]
EF1 (I need to collect information about the doctors whose services for this event might not be included in the charges on the hospital bill. I would like to record the group name, doctor name, and National Provider ID, if available.)
Physician Name: NODE.SBDDOC
GROUP/PREFIX/FIRST /MIDDLE /LAST /NTL_PROVIDER
EF3 What is this physician’s specialty?
DCS: START TYPING IN SPECIALTY TO MAKE A SELECTION.
Specialty: NODE.SBDSPEC
[IF OTHER:] Please specify the other specialty: R_NODE.OSSBDSPEC
EF2 Did this doctor provide any of the following services for this event: radiology, anesthesiology, pathology, or surgery?
SELECT ONE
1 Radiology
2 Anesthesiology
3 Pathology
4 Surgery
5 None of the above
6 DON’T KNOW
EF5 How would you describe the role of this doctor for this medical event?
SELECT ONE
SCREEN LABEL DISPLAY ORDER STORED VALUE
Active Physician/Providing Direct Care 1 6
Referring Physician 2 1
Copied Physician 3 2
Followup Physician 4 3
Department Head 5 4
Primary Care Physician 6 5
Some Other Physician 7 7
None of the above 8 8
DON’T KNOW 9 9
(IF OTHER DESCRIBE) Please describe the other role.
EF6 ENTER ANY COMMENTS ABOUT THIS SBD INCLUDING ADDITIONAL SERVICE(S) TO THE ONE PREVIOUSLY SELECTED [FILL SPECIALTY].
PROGRAMMER NOTES: SBD SUBROUTINE
2018 UPDATE: Create the ability to add notes in the system when keying SBD or any “additional information” (Example: Internal Medicine Dr serving as the Cardiologist). This information will be seen on the SBD node listing screen and master node list. This will assist the SBD DCS to probe more effectively to locate the correct SBD/data.
2018 UPDATE: On the list for SBD specialties, add Respiratory Therapy.
2017 UPDATE: Move “Previous SBD” list to the middle of the subroutine series of questions for better visibility.
2017 UPDATE: On the list for SBD specialties, add the following options.
o Occupational Therapy
o Physical Therapy
2016 UPDATE: SBD information collected to appear in alphabetical order in the SBD list.
2016 UPDATE: SBD groups to appear in the SBD list.
2016 UPDATE: The following items will be edited so that the Event Form matches the Abstraction Notes Forms:
In the list for item EF2, place #s in front of each option:
1. Radiology
2. Anesthesiology
3. Pathology
4. Surgery
5. None of the above
6. DON’T KNOW
In the list for item EF5, place #s in front of each option:
1. Active Physicians/Providing Direct Care
2. Referring Physician
3. Copied Physician
4. Followup Physician
5. Department Head
6. Primary Care Physician
7. Some Other Physician
8. None of the above
9. DON’T KNOW
This SBD subroutine in hospital event form is a loop of six (6) questions, EF1 to EF6, and a “stop command” in EF7. The subroutine collects SBD name, specialty, billing practices, and role in this particular hospital event (e.g., sometimes SBDs are just offering advice).
After the collection of the SBD name in EF1, display the name under the main header in the upper left, but above the next questions within the SBD subroutine. After the collection of specialty in EF3, display the specialty with the name in the header for remaining SBD subroutine questions about that SBD.
Launch the SBD subroutine when question A3 ANYSBDS=YES (1).
If user enters A3=NO (2) or DK or REF, A3 should remain accessible via navigation back to item A3 to allow revision of A3 to YES.
EF1: We want users to enter name of doctor or group and populate a dynamic database at the provider-level, no higher. Display three text fields for user to record the SBD’s first name, middle name or initial, and last name. Label those text fields FIRST, MIDDLE, LAST. In later event forms, the user should be able to “Select Existing SBD” and see names already entered from previous event forms. Newly added Provider ID (below last name of doctor) is 10-digits long. Move Group Name before Prefix and Name fields.
Fields include:
EF3: As one types characters in this field, EF3 should display corresponding list of specialties. For example if user starts entering “pedi…” they should see “pediatric allergy,” “pediatric cardiology,” pediatric critical care medicine,” and so on. Note the other-specify text box, R_NODE.OSSBDSPEC, to hold 50 characters. Do not require response in box. There is an enumerated option for “Unknown.”
Fields include:
EF2: “Don’t Know” is an enumerated response.
EF5: Note that Don’t Know is an enumerated response.
Note the other-specify text box, NODE.ODOCTYOS, to hold 50 characters. Do not require response in box.
Fields include:
ROLE_ASK = EF5ROLE_ASK
EF5ROLE (automatically filles based on value entered in EF5ROLE_ASK)
OTHER_ROLE = EF5ROLE_OTHER
EF6: Text box to allow 100 characters. Do not require response in box.
Field: OTHER_ROLE = EF5ROLE_OTHER
At the form level, the required fields are EF1 (Items EF1FIRST and EF1LAST), EF3 (EF3SPECIALTYDESC), EF2 (EF2SERVICE), EF5 (EF5ROLE_ASK). Other fields within EF1 are optional. EF6 is optional. User is not allowed to move beyond item EF5 for an SBD before completing the required fields FOR EF1, EF3, EF2, AND EF5.. Attempting to move past past EF5 without completing all the required elements results in the following hard check: “FIRST AND LAST NAME, SPECIALTY, SERVICE, AND ROLE ARE REQUIRED WHEN ENTERING OR UPDATING AN SBD.”
Table of Physician Specialties
General Classification from EF2 |
code |
New label for user in OY2 |
1, Radiology |
1000 |
Radiology - General |
1, Radiology |
1001 |
Radiology - Abdominal |
1, Radiology |
1002 |
Radiology - Diagnostic |
1, Radiology |
1003 |
Radiology - Neuroradiology |
1, Radiology |
1004 |
Radiology - Nuclear |
1, Radiology |
1005 |
Radiology - Pediatric |
1, Radiology |
1006 |
Radiology - Radiation Oncology |
1, Radiology |
1007 |
Radiology - Radiological Physics |
1, Radiology |
1008 |
Radiology - Radiology/Neuroradiology |
1, Radiology |
1009 |
Radiology - Vascular & Interventional Radiology |
1, Radiology |
1999 |
Radiology - Radiology Other Specify |
2, Anesthesiology |
2000 |
Anesthesiology - General |
2, Anesthesiology |
2001 |
Anesthesiology - Certified Registered Nurse Anesthesiologist (CRNA) |
2, Anesthesiology |
2002 |
Anesthesiology - Critical Care Medicine |
2, Anesthesiology |
2003 |
Anesthesiology - Medical Toxicology Preventive Medicine |
2, Anesthesiology |
2004 |
Anesthesiology - Pain Management |
2, Anesthesiology |
2005 |
Anesthesiology - Pediatric |
2, Anesthesiology |
2999 |
Anesthesiology - Anesthesiology Other specify |
3, Pathology |
3000 |
Pathology - General |
3, Pathology |
3001 |
Pathology - Allergy & Immunology / Clinical & Lab Immunology |
3, Pathology |
3002 |
Pathology - Anatomic & Clinical Pathology |
3, Pathology |
3003 |
Pathology - Anatomic |
3, Pathology |
3004 |
Pathology - Chemical |
3, Pathology |
3005 |
Pathology - Clinical & Lab Dermatological Immunology |
3, Pathology |
3006 |
Pathology - Clinical & Lab Immunology Internal Medicine |
3, Pathology |
3007 |
Pathology - Clinical & Lab Immunology Pediatrics |
3, Pathology |
3008 |
Pathology - Clinical |
3, Pathology |
3009 |
Pathology - Cytopathology |
3, Pathology |
3010 |
Pathology - Dermatopathology |
3, Pathology |
3011 |
Pathology - Forensic |
3, Pathology |
3012 |
Pathology - Hematology |
3, Pathology |
3013 |
Pathology - Molecular Genetic Pathology |
3, Pathology |
3014 |
Pathology - Neuropathology |
3, Pathology |
3015 |
Pathology - Pediatric |
3, Pathology |
3016 |
Pathology - Selective |
3, Pathology |
3999 |
Pathology - Pathology Other specify |
4, Surgery |
4000 |
Surgery - General |
4, Surgery |
4001 |
Surgery - Abdominal |
4, Surgery |
4002 |
Surgery - Adult Reconstructive Orthopedics |
4, Surgery |
4003 |
Surgery - Cardiothoracic |
4, Surgery |
4004 |
Surgery - Certified Peri Surgery Nurse (CNOR) |
4, Surgery |
4005 |
Surgery - Colon & Rectal |
4, Surgery |
4006 |
Surgery - Craniofacial |
4, Surgery |
4007 |
Surgery - Dermatologic |
4, Surgery |
4008 |
Surgery - Facial Plastic |
4, Surgery |
4010 |
Surgery - Hand |
4, Surgery |
4011 |
Surgery - Head & Neck |
4, Surgery |
4012 |
Surgery - Neurological |
4, Surgery |
4013 |
Surgery - Orthopedic |
4, Surgery |
4014 |
Surgery - Orthopedic Surgery of the Spine |
4, Surgery |
4015 |
Surgery - Pediatric Cardiothoracic |
4, Surgery |
4016 |
Surgery - Pediatric |
4, Surgery |
4017 |
Surgery - Pediatric Surgery Neurology |
4, Surgery |
4018 |
Surgery - Plastic |
4, Surgery |
4019 |
Surgery - Plastic Surgery within Head & Neck |
4, Surgery |
4020 |
Surgery - Sports Medicine Orthopedic |
4, Surgery |
4021 |
Surgery - Surgeon/Thoracic |
4, Surgery |
4022 |
Surgery - Critical Care |
4, Surgery |
4023 |
Surgery - Surgical Oncology |
4, Surgery |
4024 |
Surgery - Transplantation |
4, Surgery |
4025 |
Surgery - Traumatic |
4, Surgery |
4026 |
Surgery - Vascular |
4, Surgery |
4999 |
Surgery - Surgery Other specify |
5, Other specialty |
5000 |
Addiction Medicine |
5, Other specialty |
5001 |
Addiction Psychiatry |
5, Other specialty |
5002 |
Adolescent Medicine Internal Medicine |
5, Other specialty |
5003 |
Allergy & Immunology |
5, Other specialty |
5004 |
Audiology |
5, Other specialty |
5005 |
Blood Banking/Transfusion |
5, Other specialty |
5006 |
Cardiac Electrophysiology |
5, Other specialty |
5130 |
Cardiology |
5, Other specialty |
5008 |
Certified Nurse Midwife |
5, Other specialty |
5009 |
Certified Registered Nurse First Assistant (CRNFA) |
5, Other specialty |
5010 |
Child & Adolescent Psychiatry |
5, Other specialty |
5011 |
Child Neurology |
5, Other specialty |
5012 |
Chiropractic |
5, Other specialty |
5013 |
Clinical Biochemical Genetics |
5, Other specialty |
5014 |
Clinical Cytogenetics |
5, Other specialty |
5015 |
Clinical Genetics |
5, Other specialty |
5016 |
Clinical Molecular Genetics |
5, Other specialty |
5017 |
Clinical Neurophysiology |
5, Other specialty |
5018 |
Clinical Pharmacology |
5, Other specialty |
5019 |
Critical Care Medicine Internal Medicine |
5, Other specialty |
5020 |
Critical Care Medicine Obstetrics & Gynecology |
5, Other specialty |
5021 |
Dermatology |
5, Other specialty |
5022 |
Developmental Behavioral Pediatrics |
5, Other specialty |
5023 |
Diabetes |
5, Other specialty |
5024 |
Emergency Medicine |
5, Other specialty |
5025 |
Endocrinology, Diabetes & Metabolism |
5, Other specialty |
5026 |
Epidemiology |
5, Other specialty |
5027 |
Family Nurse Practitioner (FNP) |
5, Other specialty |
5028 |
Family Practice |
5, Other specialty |
5029 |
Forensic Psychiatry |
5, Other specialty |
5030 |
Gastroenterology |
5, Other specialty |
5031 |
General Practice |
5, Other specialty |
5032 |
General Preventive Medicine |
5, Other specialty |
5033 |
Geriatric Medicine Family Practice |
5, Other specialty |
5034 |
Geriatric Medicine Internal |
5, Other specialty |
5035 |
Geriatric Psychiatry |
5, Other specialty |
5036 |
Gynecological Oncology |
5, Other specialty |
5037 |
Gynecology |
5, Other specialty |
5038 |
Hematology Internal Medicine |
5, Other specialty |
5039 |
Hematology/Oncology |
5, Other specialty |
5040 |
Hepatology |
5, Other specialty |
5041 |
Hospital Rounders/Hospitalist |
5, Other specialty |
5042 |
Immunology |
5, Other specialty |
5043 |
Infectious Diseases |
5, Other specialty |
5044 |
Infertility |
5, Other specialty |
5045 |
Internal Medicine |
5, Other specialty |
5046 |
Internal Medicine/Pediatrics |
5, Other specialty |
5047 |
Interventional Cardiology |
5, Other specialty |
5048 |
Legal Medicine |
5, Other specialty |
5049 |
Licensed Alcohol and Drug Counselor (LADC) |
5, Other specialty |
5050 |
Licensed Professional Counselor (LPC) |
5, Other specialty |
5051 |
Maternal & Fetal Medicine |
5, Other specialty |
5052 |
Medical Genetics |
5, Other specialty |
5053 |
Medical Management |
5, Other specialty |
5054 |
Medical Microbiology |
5, Other specialty |
5055 |
Medical Oncology |
5, Other specialty |
5056 |
Medical Toxicology Emergency Medicine |
5, Other specialty |
5057 |
Medical Toxicology Pediatrics |
5, Other specialty |
5058 |
Medicine Emergency Medicine |
5, Other specialty |
5059 |
Medicine Pediatrics |
5, Other specialty |
5060 |
Mental Health |
5, Other specialty |
5061 |
Molecular Genetic Pathology (Medical Genetics) |
5, Other specialty |
5062 |
Musculoskeletal Oncology |
5, Other specialty |
5063 |
Adolescent Medicine Pediatrics |
5, Other specialty |
5064 |
Aerospace Medicine |
5, Other specialty |
5065 |
Allergy |
5, Other specialty |
5066 |
Neonatal Perinatal Medicine |
5, Other specialty |
5067 |
Nephrology |
5, Other specialty |
5068 |
Neurodevelopmental Disabilities (Pediatrics) |
5, Other specialty |
5069 |
Neurodevelopmental Disabilities (Psychiatry) |
5, Other specialty |
5070 |
Neurology |
5, Other specialty |
5071 |
Neurology/Diagnostic |
5, Other specialty |
5072 |
Nuclear Medicine |
5, Other specialty |
5073 |
Nurse Practitioner (NP) |
5, Other specialty |
5074 |
Nutrition |
5, Other specialty |
5075 |
OB Advanced RN Practitioner (ARNP) |
5, Other specialty |
5076 |
Obstetrics |
5, Other specialty |
5077 |
Obstetrics & Gynecology |
5, Other specialty |
5078 |
Occupational Medicine |
5, Other specialty |
5132 |
Occupational Therapy |
5, Other specialty |
5079 |
Oncology |
5, Other specialty |
5080 |
Ophthalmology |
5, Other specialty |
5081 |
Orthopedic Trauma |
5, Other specialty |
5082 |
Orthopedics |
5, Other specialty |
5083 |
Osteopathic Manipulative Medicine Foot & Ankle |
5, Other specialty |
5131 |
Osteopathy |
5, Other specialty |
5085 |
Otology |
5, Other specialty |
5086 |
Pain Management (Physical Medicine & Rehabilitation) |
5, Other specialty |
5087 |
Pain Medicine |
5, Other specialty |
5088 |
Palliative Medicine |
5, Other specialty |
5089 |
Pediatric Allergy |
5, Other specialty |
5090 |
Pediatric Cardiology |
5, Other specialty |
5091 |
Pediatric Critical Care Medicine |
5, Other specialty |
5092 |
Pediatric Emergency |
5, Other specialty |
5093 |
Pediatric Endocrinology |
5, Other specialty |
5094 |
Pediatric Gastroenterology |
5, Other specialty |
5095 |
Pediatric Hematology Oncology |
5, Other specialty |
5096 |
Pediatric Infectious Diseases |
5, Other specialty |
5097 |
Pediatric Nephrology |
5, Other specialty |
5098 |
Pediatric Ophthalmology |
5, Other specialty |
5099 |
Pediatric Orthopedics |
5, Other specialty |
5100 |
Pediatric Otolaryngology |
5, Other specialty |
5101 |
Pediatric Pulmonology |
5, Other specialty |
5102 |
Pediatric Rehabilitation Medicine |
5, Other specialty |
5103 |
Pediatric Rheumatology |
5, Other specialty |
5104 |
Pediatric Urology |
5, Other specialty |
5105 |
Pediatrics |
5, Other specialty |
5106 |
Pharmaceutical Medicine |
5, Other specialty |
5107 |
Physiatrist |
5, Other specialty |
5108 |
Physical Medicine & Rehabilitation |
5, Other specialty |
5133 |
Physical Therapy |
5, Other specialty |
5109 |
Physicians Assistant (PA, PAC) |
5, Other specialty |
5110 |
Podiatry |
5, Other specialty |
5111 |
Preventive Medicine Public Health & Gen Prev Med |
5, Other specialty |
5112 |
Proctology |
5, Other specialty |
5113 |
Psychiatry |
5, Other specialty |
5114 |
Psychoanalysis |
5, Other specialty |
5115 |
Pulmonary Critical Care Medicine |
5, Other specialty |
5116 |
Pulmonary Diseases |
5, Other specialty |
5117 |
Reproductive Endocrinology |
5, Other specialty |
5135 |
Respiratory Therapy |
5, Other specialty |
5118 |
Rheumatology |
5, Other specialty |
5119 |
Sleep Medicine |
5, Other specialty |
5134 |
Sleep Therapy |
5, Other specialty |
5120 |
Spinal Cord Injury |
5, Other specialty |
5121 |
Sports Medicine (Physical Medicine & Rehabilitation) |
5, Other specialty |
5122 |
Sports Medicine Emergency Medicine |
5, Other specialty |
5123 |
Sports Medicine Family Practice |
5, Other specialty |
5124 |
Sports Medicine Internal Medicine |
5, Other specialty |
5125 |
Sports Medicine Pediatrics |
5, Other specialty |
5126 |
Undersea Medicine & Hyperbaric Medicine |
5, Other specialty |
5127 |
Urgent Care |
5, Other specialty |
5128 |
Urology |
5, Other specialty |
5129 |
Vascular Medicine |
5, Other specialty |
5999 |
Other Unclassified Specialty |
5, Other specialty |
6999 |
EDIT SPECS FROM WESTAT
QA3 ANY SBDs? Follow Skip Pattern
-
DATA ITEM
SPECIFICATIONS
ACTION, if specification not met
QA3 – Any Separately Billing Doctors for this event?
Must be answered.
1 – YES, there are Separately Billing Doctors for this event
2 – NO, there are no SBDs for this event
Live SBDs must have the Billing Status box BILLS SEPARATELY checked on the SBD form.
If CHARGES ARE INCLUDED IN HOSPITAL BILL is checked on the SBD form, do not count this form as a live SBD.
If no Billing Status box is checked on the SBD form – if the SBD form is completed, check the BILLS SEPARATELY box and count this form as a live SBD.
ONLY THE TRC CAN CIRCLE 2 (NO SBDs).
If blank, review SBD forms. Do any dates on an SBD form match this event?
If blank
If the event date appears on a live SBD form for this event, write answer YES (1), THERE ARE SBDs.
If QA3 is blank
And no SBD for this event, Blue Sheet, saying “QA3 is not answered.”
I4 CASES HAVE NO SBDs. IF ALL PAIRS IN THE CASE ARE CODED I4, FOLLOW THE INSTRUCTIONS ON THE “I4 = NO SBDs REFERENCE SHEET.
In I4 cases, QA3 should be 2 (NO SBDs).
If the answer is 1 – SEPARATELY BILLING DOCTORS FOR THIS EVENT
There must be a live SBD for this event.
This is true for all cases, even I4 cases which usually don’t have SBDs.
Blue Sheet, if answered “1” but no live SBD for this event.
Every event book with the answer “1” must have a live SBD. Blue Sheet, even if the case is an I4.
If the answer from the TRC is 2 –NO SEPARATELY BILLING DOCTORS FOR THIS EVENT
There should be no live SBD for this event.
Editors can change NO to YES, but ONLY THE TRC CAN CIRCLE 2 (NO SBDs).
Change 2 (NO) to 1 (YES) if there is a live SBD form.
SBD forms that are crossed out because “Charges are included in Hosp bill” cannot be counted as Separately Billing Doctors for the QA3 answer.
DK or RF needs managerial review.
Yellow Sheet.
Notes on inside cover account for expected SBDs.
If the case is NOT an I4 –
All cases except I4 cases must be reviewed to identify what SBDs would be expected.
Look for S, A, P, R, ER
The TRC writes notes across from QA3 to indicate why an expected SBD is missing.
As you edit the rest of the booklet, determine what specialties would be expected to provide service.
Record the initials of the expected specialty on the front cover.
Account for the specialty by reviewing SBD forms and TRC documentation.
I4 cases do not need notes to account for expected specialties.
Follow the instructions on the I4 reference sheet to make sure that the case follows the I4 criteria.
Write “I4 on the cover of the book, in place of the abbreviations for needed SBDs. Do not determine which SBDs are needed.
SECTION 6 – MEDICAL RECORDS – Diagnoses
[Page 7 – MEDICAL RECORDS - Diagnoses (1 of 1)]
ScreeN LAYOUT
A4a.CODE I need the diagnoses for (this stay/this visit). I would prefer the ICD-10 codes or DSM-5 codes, if they are available.
IF CODES ARE NOT USED, RECORD DESCRIPTIONS.
RECORD UP TO FIVE ICD-10 CODES OR DESCRIPTIONS
A4a. DESCRIPTION I need the diagnoses for this (stay/visit).
ENTER DESCRIPTION |
ICD-10 CODE DESCRIPTION ICDCND# ICDPDS# ICDCND# ICDPDS# ICDCND# ICDPDS# ICDCND# ICDPDS# ICDCND# ICDPDS#
|
PROGRAMMER NOTES
[SYSTEM SHOULD ALLOW FOR A MAXIMUM OF 5 ICD-10 CODES TO BE COLLECTED]
(this stay/these visit) - If MREVTYPE (A1)=1 or 5, fill: "this stay" ELSE fill: "this visit".
This is a question loop that will require:
A HISTORY BOX to display responses already collected.
A question to appear after each iteration of the questions that reads: Any More Diagnoses? YES=1 NO=2
DK/REF – CONTINUE TO A5a
For ICDCND, display “ENTER CODE” on screen. For ICDPDS, display “ENTER DESCRIPTION” on screen.
Description field allows up to 100 characters.
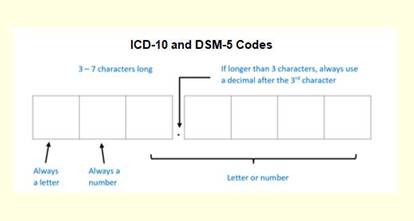
2019 UPDATE: Addition of onscreen ICD-10 graphic to emphasize correct code format. Logic also added to restrict code entries to only accurate formats.
Code is 3-7 characters.
First character is always a letter.
Second character is always a number.
Characters 3-7 can be letter or number.
2020 UPDATE: Values entered into ICDCND are checked against a dictionary of valid ICD-10 and DSM-5 codes. Entry is allowed for valid codes. If entry of an invalid code is attempted, a hard check message is displayed, “The code you entered is not in our database. Please verify your entry. If the entry is correct, leave ICDCND empty and move to ICDPDS field to enter a description instead.”
SBD REAL-TIME PROMPTING
OVERVIEW: If A4a collects a code in ICDCND# or text in ICDPDS# that is associated with certain expected SBDs (see list below STEP 3), but no such SBD was described in EF2, the system will prompt the respondent in real time with questions SBDPR1-SBDPR3. Those ask whether respondent overlooked SBDs in the medical record.
STEP 1: Upon collecting ICD code (ICDCND#) or description (ICDPDS#) then the system should set “expectation flags” for surgery, anesthesiology, pathology, radiology. Flag names are R_SPECTYPE_R (radiology), R_SPECTYPE_A (anesthesiology), R_SPECTYPE_P (pathology), and R_SPECTYPE_S (surgery). Flag values are by default 0, or set to 1 based on reported ICD code or description.
EXAMPLE 1: ICDCND# records a code of 91.6, which means microscopic examination of skin sample. That would set the flag to R_SPECTYPE_P = 1 because such a procedure implies an SBD trained in pathology was involved.
EXAMPLE 2: ICDPDS# records ”fluoroscopy” and R_SPECTYPE_R = 1 because such a procedure implies an SBD trained in radiology was involved.
EXAMPLE 3: ICDPDS# records “high fever and delirium” and no flag is set because those text phrases are not among those we are tracking in the list below STEP 3.
STEP 2: If R_SPECTYPE_S is set to “1” based on A4a responses, then system will check EF2 to see if it recorded specialties of Surgery (4), Anesthesiology (2), and Pathology (3) because those three specialties of SBDs often associated with surgery.
If R_SPECTYPE_A is set to “1” based on responses to A4a, system will check EF2 to see if we have recorded an SBD specialty = Anesthesiology (2).
If R_SPECTYPE_P is set to “1” based on responses to A4a, system will check EF2 to see if we have collected an SBD specialty = Pathology (3).
If R_SPECTYPE_R is set to “1” based on responses to A4a, system will check EF2 to see if we have collected an SBD specialty = Radiology (1).
STEP 3: If STEP 2 determines we are not missing any expected specialty of SBDs, then go to A5a.
STEP 4: If STEP 2 determines we are missing one or more specialty, then SBDPR1 to SBDPR3 below administer as needed for each missing specialty to prompt respondents to re-check medical records.
SBDPR1: A diagnosis that you mentioned often involves a (FILL SPECIALTY). We did not record such persons in the earlier questions about separately billing doctors. Did you not mention them for this patient event because they were residents or interns?
IF SPECIALTY RECORDED IN COMMENTS, ANSWER “NO” HERE.
YES=1
NO=2
SBDPR1 PROGRAMMING NOTES
FILL SPECIALTY = “surgeon,” “anesthesiologist,” and “pathologist” when R_SPECTYPE_S=1
FILL SPECIALTY = “anesthesiologist” when R_SPECTYPE_A=1
FILL SPECIALTY = “pathologist” when R_SPECTYPE_P=1
FILL SPECIALTY = “radiologist” when R_SPECTYPE_R=1
If SBDPR1=YES, SKIP TO A5a
If SBDPR1=NO, ASK SBDPR2
SBDPR2: Do your records indicate that a (FILL SPECIALTY) was associated with this patient event?
IF SPECIALTY RECORDED IN COMMENTS, ANSWER “NO” HERE.
YES=1
NO=2
SBDPR2 PROGRAMMING NOTES
FILL SPECIALTY = “surgeon,” “anesthesiologist,” and “pathologist” when R_SPECTYPE_S=1
FILL SPECIALTY = “anesthesiologist” when R_SPECTYPE_A=1
FILL SPECIALTY = “pathologist” when R_SPECTYPE_P=1
FILL SPECIALTY = “radiologist” when R_SPECTYPE_R=1
If SBDPR2=YES, SYSTEM SKIP FOCUS BACK TO A3 via hard check: IF YES, GO BACK TO A3 AND THE SBD SELECTION SCREENS IN ORDER TO ACCOUNT FOR THE MISSING SBD FOR (FILL SPECIALTY). HIGHLIGHT ‘SBD.ANYSBDS’ BELOW, THEN CLICK ON THE ‘Goto’ BUTTON TO MOVE TO A3.
If SBDPR2=NO, GO TO SBDPR3
SBDPR3: PROBE WHY THERE WAS NO SBD OF THE EXPECTED TYPES FOR THIS EVENT
IF SPECIALTY RECORDED IN COMMENTS, NOTE THAT HERE.
.
Create a text box that allows 100 characters.
ICD-10 CODES ASSOCIATED WITH SBDS (VARIABLE NAME ICDCND#)
*NOTE ALL SURGERY RELATED CODES WILL ALSO PROMPT FOR ANESTHESIOLOGY AND PATHOLOGY
ICD10 |
Text |
Surg |
Anest |
Path |
Rad |
Other |
ICD9 |
NA |
procedure codes |
|
|
|
|
|
01.0-86.99 |
I46.9 |
Cardiac arrest |
|
|
|
Y |
Cardiologist, ER physician |
427.5 |
I51.1 |
Rupture of chordae tendineae |
Y |
Y |
Y |
Y |
Cardiologist |
429.5 |
I51.2 |
Rupture of papillary muscle |
Y |
Y |
Y |
Y |
Cardiologist |
429.6 |
J95.00 |
Tracheostomy complications |
|
|
|
|
ER physician, pulmonologist |
519 |
K11.3 |
Abscess of salivary gland |
Y |
Y |
Y |
Y |
|
527.3 |
P00.6/P00.7 |
Surgical operation on mother and fetus |
Y |
Y |
Y |
|
Neonatologist, OB-GYN |
760.6 |
S11 |
Open wound of neck |
Y |
Y |
Y |
|
ER physician, pulmonologist |
874 |
NA |
Open wound of genital organs (external) including traumatic amputation |
Y |
Y |
Y |
Y |
Gynecologist/urologist (depending on sex), neurologist |
878 |
T30.0 |
Burn unspecified site |
Y |
Y |
Y |
Y |
ER physician, neurologist, plastic surgeon |
949 |
T41.44 |
Poisoning by other central nervous system depressants and anesthetics |
|
Y |
Y |
|
Neurologist |
968 |
S40 - S69 |
Traumatic amputation of thumb (complete) (partial), Traumatic amputation of other finger(s) (complete) (partial),Traumatic amputation of arm and hand (complete) (partial) |
Y |
Y |
Y |
Y |
ER physician, neurologist |
885-7 |
S88, S98 |
Traumatic amputation of toe(s) (complete) (partial), Traumatic amputation of foot (complete) (partial), Traumatic amputation of leg(s) (complete) (partial) |
Y |
Y |
Y |
Y |
ER physician, neurologist |
895-7 |
T80-T88 |
Complications Of Surgical And Medical Care, Not Elsewhere Classified |
Y |
Y |
Y |
Y |
|
996-9 |
Z41.1 |
Elective hair transplant for purposes other than remedying health states, Other plastic surgery for unacceptable cosmetic appearance |
Y |
Y |
Y |
|
Plastic surgeon |
V50-1 |
O74.9 |
Complications of the administration of anesthetic or other sedation in labor and delivery |
|
Y |
|
|
Cardiologist, neurologist, OB-GYN, pulmonologist |
668 |
P02.9 |
Fetus or newborn affected by complications of placenta cord and membranes |
Y |
Y |
Y |
|
Neonatologist, OB-GYN, pediatrician |
762 |
P03.9 |
Fetus or newborn affected by other complications of labor and delivery |
Y |
Y |
Y |
|
Neonatologist, neurologist, OB-GYN, pediatrician |
763 |
Z37.9 |
Outcome of delivery |
Y |
Y |
Y |
|
Neonatologist, OB-GYN, pediatrician |
V27 |
NA |
procedure codes |
|
|
|
|
|
90.0-91.9 |
D58.9 |
Hereditary hemolytic anemias |
|
|
Y |
|
Hematologist |
282 |
D64.89, D64.9 |
Other and unspecified anemias |
|
|
Y |
|
Hematologist |
285 |
D72.9 |
Diseases of white blood cells |
|
|
Y |
|
Hematologist |
288 |
O99.119 |
Coagulation defects complicating pregnancy, childbirth, or the puerperium |
|
|
Y |
|
Hematologist, neonatologist, OB-GYN, pediatrician |
649.3 |
O99.350 |
Epilepsy complicating pregnancy, childbirth, or the puerperium |
|
|
|
Y |
Neonatologist, neurologist, OB-GYN, pediatrician |
649.4 |
ICD-10 TEXT ASSOCIATED WITH SBDS (VARIABLE NAME ICDPDS#)
*NOTE ALL SURGERY RELATED TEXT WILL ALSO PROMPT FOR ANESTHESIOLOGY AND PATHOLOGY
Surgery: surg*, excision, removal, incision, introduction, repair, operat*, biopsy, recovery, delivery, graft, transplant, *oscopy, EGD, ERCP, dilation, courettage, *ectomy, *ostomy, *oplasty, *rrhaphy,
Anesthesiology: anesth*, block, local
Pathology: pathol*, test, lab*, finding, biopsy, result, -puncture, draw, culture, chemistry, micro*, cytology, panel, profile, hemoglobin, hematology, cholesterol, lipid, lipoproteins, assay, antibody, screen, blood gases, smear, stain, occult blood, count, hematocrit, re-agent, transfusion, blood bank, blood sugar, A1C, ABD, AFB, thrombo*, APTT, BMP, bleeding time, BT, blood urea, BUN, C & S, CBC, sensitivity, creatine, CK, CMP, dilation, courettage, D & C, ERA, FBS, Hb, lipoprotein, HDL, LDL, volume, MCV, MPV, OB, PAP, PKU, phenyl*, TB, PPD, PSA, antigen, prothrombin, PT, PTT, RBC, RDW, red cell, T & S, type, TSH, thyroid, UA, WBC, *alysis
Radiology: Radiolog*, ultra*, MRI, *scan, *gram, x-ray, imaging, diagnostic, nuclear, compute*, tomography, magnetic, resonance, fluoroscopy, *raphy, abdomen, wrist, upper GI, angio*, barium, techni*, roentgen, anterior*, posterior, AP, Ba, BaE, enema, CAT, C-spine, CT, axial, film, DSA, ERCP, endoscop-, radiation, ERT, Fx, fracture, GB, IRT, IVC, IVP, intravenous, KUB, kV, kW, kilo*, lateral, Lat, LGI, LL, NMR, PA, PET, emission, Ra, Rad, RL, UGI, UL, US, *graph
2019 Update: The following terms from the lists above will result in a prompt for SBDs only when the terms are stand-alone terms, and not part of a larger word or term.
PA, RA, US, CT, UL, LL, BA, ERA, CK, ERT, OB, LAT, CAT, RL, AP, ABD
These short terms are excluded from resulting in a prompt for SBDs based on the following process:
Process first searches for the existence of the small string within a larger string. If exists:
Searches beginning of larger string for existence of smaller string plus space or other special character placed after it. Examples: "ct ", "ct-"
Searches end of larger string for existence of smaller string plus space or other special character placed before it. Examples: " ct", ":ct"
Searches larger string for existence of smaller string with combinations of special characters surrounding it. Examples: " ct ", "(ct ", " ct/", "(ct)", "[ct ", "+ct;", "_ct."
If one of the short terms is found through these searches to be a stand-alone term, it is allowed to result in the prompt for an SBD, as appropriate. If it is found to be part of a larger word/term, it is excluded from resulting in a prompt for an SBD.
Special characters involved in steps 1a-1c are:
(hyphen)
(
)
_ (underscore)
+
‘
“
<
>
:
;
/
\
[
]
{
}
, (comma)
. (period)
EDIT SPECS FROM WESTAT
QA4a DIAGNOSIS
Diagnosis is a Critical Item Follow Skip Pattern
-
DATA ITEM
SPECIFICATIONS
ACTION, if specification not met
QA4a – Diagnosis
CRITICAL ITEM
USED FOR DETERMINING SBDs
Must have at least one Diagnosis, in text or code.
Blue Sheet.
DK and RF are acceptable answers.
Change DK to –8. Change RF to –7.
Code PL-IV as 60, critical item is DK or RF.
If one Diagnosis is given and another is DK, cross out the DK and keep the Diagnosis given.
Diagnosis descriptions must be valid, clear, and legible.
Blue Sheet
Diagnosis descriptions may be the identification of a disease or illness.
Symptoms are acceptable for Diagnosis.
Procedures are acceptable for Diagnosis.
Accept the name of a disease.
Accept symptoms such as cough or nausea.
Accept procedures such as lab work, screening mammogram, flu shot, employment physical, or school physical.
Do not accept “Follow-up” without any other information. Blue Sheet, asking Follow-up for what.
Abbreviations in the Description field should be standard medical abbreviations.
Review abbreviations.
Check reference list in manual.
Check medical dictionary.
Ask team leader to check website.
Yellow Sheet, if not found, and team leader is not available.
There should be only 1 diagnosis per line.
If there are 5 or more codes, the order of the codes must be maintained.
Change
To
Change
To
650 652
V27.1
V25.2
V25.09
650
652
V27.1
V25.2
V25.09
650 652
V27.1
V25.2
650
V27.1
V25.2
652
If two codes are listed on the same line, rewrite one of the codes.
If there are 4 or less Diagnoses, write the code on the last line.
If there are 5 or more Diagnoses, write the code on the next line and rewrite all other codes, keeping them in order.
The code field and the description field cannot be used on the same line.
CODE DESCRIPTION
650
Normal Delivery
A mixture of codes and descriptions are acceptable if they are on different lines.
CODE DESCRIPTION
650 _____________
____ Normal Delivery
Look up the diagnosis code in the ICD-10 reference book.
If they are on the same line, and the code’s definition exactly matches the text description, cross out the text and keep the code. Do not look up codes if they are on different lines.
If there are 5 or more Diagnoses, write the code on the next line and rewrite all other codes, keeping them in order
QA4a– Diagnosis, cont.
CRITICAL ITEM
USED FOR DETERMINING SBDs
A diagnosis may only appear in the book once.
Note: different numbers after the decimal mean that a diagnosis is not a duplicate. Keep both.
547.11 and 547.1 are not duplicates.
698 and 698.0 are not duplicates.
Cross out a duplicate diagnosis.
If the number of diagnoses is greater than 4, a continuation sheet may be used.
Staple the continuation sheet to the top of Page 2.
If extra diagnoses were written without a continuation sheet, make sure that they are legible for Cading, or rewrite them on a continuation sheet.
Descriptions cannot go over 100 characters.
Take to a team leader to shorten, or write a Yellow Sheet.
Some sequential events will have ongoing treatments for a condition.
Pre-natal care
Dialysis
Physical or Occupational Therapy
If diagnosis is given in some books, but DK or RF in other books, managerial review is needed
Yellow Sheet, if diagnosis is given in some books, but is DK or RF in other books.
Diagnosis Counter
Office Use Only box must be filled in.
The Office Use Only box is only used on the booklet page, not on the Continuation Sheet.
Count the number of diagnoses and enter as a 2-digit, zero-filled number.
Diagnosis of DK or RF = Diagnosis count of 01.
CHEAT SHEET RANGES FOR DIAGNOSES (ICD-10)
Codes are between 3 and 7 characters, ranging from A00 to Z99.

SECTION 9 – PATIENT ACCOUNTS – Global Fee
NOTE: See end of section for edit specs from Westat for questions A5a, A5b, A5c, A5d, and A5e.
[Page 9 – PATIENT ACCOUNTS - Global fee (1 of 4)]
ScreeN LAYOUT
GLOBAL FEE |
|
A5a. Was the visit on that date covered by a global fee, that is, was it included in a charge that covered services received on other dates as well?
EXPLAIN IF NECESSARY: An example would be a patient who received a series of treatments, such as chemotherapy, that was covered by a single charge.
PROGRAMMER NOTES IF GLOFEE=2 GO TO A6a. DK/REF – GO TO A6a |
YES=1, NO=2 GLOFEE
|
[Page 10 – PATIENT ACCOUNTS - Global fee (2 of 4)]
ScreeN LAYOUT
A5b. Did the global fee for this date cover any services received while the patient was an inpatient? PROGRAMMER NOTES IF GFEECOVS = 2 GO TO A5d. DK/REF – GO TO A5d |
YES=1, NO=2 GFEECOVS
|
[Page 11 – PATIENT ACCOUNTS - Global fee (3 of 4)]
ScreeN LAYOUT
A5c. What was the admit date of that stay?
What was the discharge date of that stay?
REFERENCE PERIOD – CALENDAR YEAR 2022 ENTER A DATE IN FORMAT MM/DD/YYYY. INCLUDE LEADING 0’s FOR SINGLE DIGIT MONTHS AND DAYS. CODE AS “9/9/9999” IF NOT YET DISCHARGED.
PROGRAMMER NOTES IF A2c = NOT YET DISCHARGED, ENTER DISCHARGE AS 9/9/9999.
GFEEBEG_DATE – value for month should be between 1 and 12 GFEEBEG_DATE – value for day (DD) should only valid numbers (1-28 for all months; 29-30 for all months except month 2; 31 allowed only for months 1, 3, 5, 7, 8, 10, and 12; value 29 allowed for month 2 only in leap years) GFEEBEG_DATE – value for year should be 2021 or 2022 (Add soft check for 2021 “WARNING - You have entered a year other than study year. Please review and correct if needed, or suppress and continue.”) (Add hard check for years other than 2021 or 2022 “YEAR MUST BE 2022, PLEASE CORRECT”) GFEEEND_DATE – value for month should be between 1 and 12 GFEEEND_DATE – value for day (DD) should only valid numbers (1-28 for all months; 29-30 for all months except month 2; 31 allowed only for months 1, 3, 5, 7, 8, 10, and 12; value 29 allowed for month 2 only in leap years) GFEEEND_DATE – value for year should be 2022 or 2023 (Add soft check for 2023 “WARNING - You have entered a year other than study year. Please review and correct if needed, or suppress and continue.”) (Add hard check for years other than 2022 or 2023 “YEAR MUST BE 2022, PLEASE CORRECT”)
DK/REF – CONTINUE TO A5d
|
ADMIT: GFEEBEG_DATE
DISCHARGE: GFEEEND_DATE
|
[Page 12 – PATIENT ACCOUNTS - Global fee (4 of 4)]
ScreeN LAYOUT
A5c1. Were there any other dates on which services were covered by this global fee? 1 YES 2 NO A5d. What were the other dates on which services covered by this global fee were provided? Please include dates before or after 2022 if they were included in the global fee.
ENTER A DATE IN FORMAT MM/DD/YYYY. INCLUDE LEADING 0’s FOR SINGLE DIGIT MONTHS AND DAYS.
Did (PATIENT NAME) receive services on this date in an:
Outpatient Department (TYPE=OP) Emergency Room (TYPE=ER) Somewhere else (TYPE=96)
Specify the other location where services were received.
|
GFEEOTHRS_1
A5_EVNTBEG_DATE
GFTYPETXT
A5_WHSPC IF TYPE=91, SPECIFY A5_WHSPC_OTH
|
A5e. Do you expect (PATIENT NAME) will receive any future services that will be covered by this same global fee?
|
YES=1, NO=2 GFEEFUTS
|
A5f. You’ve described different dates of service covered by a global fee. Do you know if there were additional doctors providing services whose charges weren’t included in the hospital bill? |
YES=1, NO=2 GFEEDOC |
PROGRAMMER NOTES
A5c1 – “NO” GO TO A5e
DK/REF NOT ALLOWED
A5d - [SYSTEM WILL SET UP AS A LOOP, SO NO LIMIT ON NUMBER OF DATES REQUIRED]
A5_EVNTBEG_DATE – value for month should be between 1 and 12
A5_EVNTBEG_DATE – value for day (DD) should only valid numbers (1-28 for all months; 29-30 for all months except month 2; 31 allowed only for months 1, 3, 5, 7, 8, 10, and 12; value 29 allowed for month 2 only in leap years)
A5_EVNTBEG_DATE – value for year may be 2021, 2022, or 2023. (Add soft check for 2021 and 2023 “You have entered a year other than study year. Press Cancel to make a correction or OK to continue.”) (Add hard check for years other than 2021, 2022, or 2023: “YEAR MUST BE 2022, PLEASE CORRECT”).
A5d is a question loop that will require:
A HISTORY BOX to display responses already collected.
A question to appear after each iteration of the questions that reads: Any More Dates? YES=1 NO=2
If 96 (“Somewhere else”) (displays onscreen as option 3) is entered for GTYPETXT, GO TO A5_WHSPC. Response options for A5_WHSPC are: Ambulance; Hospital Free Standing Clinic/ Hospital Satellite Clinic; Independent Facility; Independent Pathology Clinic, Laboratory, Clinical Lab; Independent Radiology Clinic, Imaging CTR, X-Ray; Institution; Long Term Care Unit; Observation, Ambulatory Surgery Center; Rehab Center; SNF; SurgiCenter; Other.
If Other (91) is selected for A5_WHSPC, provide a text box for the DCS/abstractor to enter the “specify” option.
The “specify” option should be set up so a response can be entered in as text in item A5_WHSPC_OTH. The text box allows up to 50 characters.
At A5d and A5e, (PATIENT NAME) should fill with patient’s first name and patient’s last name from Housing Component data file.
A5d - DK/REF – CONTINUE TO A5e
A5e - DK/REF –CONTINUE TO A5f.
A5f –IF GFEEDOC = 1, DISPLAY HARD CHECK. IF GFEEDOC = 2, DK/RF go to a6A. hARD CHECK SAYS “if YES, go back to a3 and the sbd selections screens in order to account for the missing doctor(s). highlight ‘sbd.anysbds’ below, then click on the ‘goto’ button to move to a3.”
EDIT SPECS FROM WESTAT
GLOBAL FEE SECTION Follow Skip Pattern
-
DATA ITEM
SPECIFICATIONS
ACTION, if specification not met
QA5a – Global fee or not
Cannot be blank; either 1 or 2 must be circled.
If there is a global fee date, Circle 1 (YES) if blank. If there is a global fee date and 2 (NO is answered, change to 1 (YES).
If blank, circle 2 (No), if there is no indication of a Global Fee.
DK or RF need managerial review.
Yellow Sheet.
If NO, other global fee questions are skipped.
Go to QB3.
ALL GLOBAL FEES NEED YELLOW SHEETS.
If YES, and rest of Global Fee section is filled in, send for managerial review.
Yellow Sheet.
If YES, Global Fee section must be filled in.
Blue Sheet.
If YES, Box 3 must be answered GLOBAL FEE SITUATION (1).
Check Box 3. Circle 1, if blank or if another answer is given.
QA5b – Did the Global Fee include inpatient services?
1 or 2 must be circled if QA5a is YES.
If blank, and there is no indication that there is an inpatient stay involved, Circle 2 for NO.
If YES, needs managerial review.
Yellow Sheet.
QA5c – What were the admit and discharge dates of GF inpatient stay?
Must be answered if QA5b is YES.
Blue Sheet.
QA5d Global Fee dates
Global Fee dates are not critical items. RC code will remain 63.
Year 2021, 2022, and 2023 are acceptable as Global Fee dates.
Blue Sheet.
Year cannot be DK or RF.
Blue Sheet to verify that the year is not available.
Month or Day can be DK or RF, if year is given.
Change DK to –8. Change RF to –7.
Entire Date or series of dates may not be DK or RF. (TRC indicates that there were global fee dates, but the DOS were unknown.)
Blue Sheet asking if we can get at least the year.
If date is a duplicate of any event book date, any other global fee date or any repeat visit date, it needs managerial review.
Yellow Sheet.
QA5d Global Fee event types
Each global fee date must have an event type; type cannot be blank.
Blue Sheet.
Type must be HS, OP, ER or 96.
If 96, Yellow Sheet, if the Other/Specify answer is not on the Decision Log.
If 96 (Somewhere else) is answered, there must be an answer on the SPECIFY line. Answer may be in the form of a comment outside the line.
Blue Sheet, if 96 is answered and Specify line is blank.
Answer on the SPECIFY LINE needs review.
Sometimes the answer is written outside the line, as a comment. It may be added to the line if the Decision Log instructs.
Check Decision log for all Specify answers.
If it is on the Decision log, follow directions given there.
If the answer is not there, Yellow Sheet.
Type may be DK or RF.
Change DK to – 8.
Change RF to –7.
Global Fee Counter
If Global Fee is YES, Office Use Only Box must be filled.
Count the number of global fee dates and enter them as a two-digit, zero-filled number.
If Global Fee is NO, Office Use Only box will be skipped.
Leave Office Use Only box blank.
QA5e – Future Global Fee dates expected
1 or 2 must be circled. May not be blank.
If blank and there is no indication that there will be future service, circle 2 for NO.
Should not be DK or RF.
Circle 2 for NO.
If YES, needs managerial review.
Yellow Sheet.
Decision Log
PROGRAMMER NOTES: Include all “Problems” in a drop down menu at the other specify entry of A5d and program the required “decision” behind the scenes
Question - Form Type |
Problem |
Decision / Categorization |
QA5d - Global fee event type |
Observation |
Code GF as OP |
|
Ambulatory Surgery Center |
Code GF as OP |
|
SurgiCenter |
Code GF as OP |
|
Independent Radiology Clinic, Imaging CTR, X-Ray |
Code GF as OP |
|
Independent Pathology Clinic. Laboratory, Clinical Lab |
Code GF as OP |
|
Independent Facility |
Code GF as OP |
|
Ambulance |
Yellow Sheet |
|
SNF |
Code GF as HS |
|
Rehab Center |
Code GF as HS |
|
Hospital Free Standing Clinic/ Hospital Satellite Clinic |
Code GF as OP |
|
Long Term Care Unit |
Code GF as 96 and keep as Specify answer |
|
Institution |
Code GF as 96 and keep as Specify answer |
|
Comment indicates one of the above answers |
Code following the
directions above; Change answer following the directions above
if the TRC has answered something else. |
SECTION 10 - PATIENT ACCOUNTS – SERVICES/CHARGES – OUTPATIENT/ER/OTHER
NOTE: See end of section for edit specs from Westat for questions A6a, A6b, and C2.
[Page 13 – PATIENT ACCOUNTS - SERVICES/CHARGES – OUTPATIENT/ER/OTHER (1 of 2)]
C2. [I show the total charges as OUT_TOTLCHRG / I show the charge as undetermined. / I show the charge as OUT_TOTLCHRG, although one or more charges are missing ] Is that correct?
IF INCORRECT, CORRECT ENTRIES SHOWN ABOVE AS NEEDED |
$ OUT_TOTLCHRG
|
PROGRAMMER NOTES
2021 UPDATE: Check MCPT fields for any of the following codes or modifiers:
HCPCS/CPT4 codes: G0425, G0426, G0427, G0406, G0407, G0408, G2012, G2010, 99421, 99422, 99423, G2061, G2062, G2063
2022 UPDATE: Add the following HCPCS/CPT4 codes: 99441, 99442, 99443, 98966, 98967, 98968Modifiers: 95, GQ, GT
Determine YES or NO if any of the codes or modifiers listed immediately above are in MCPT fields. If NO, no soft check is displayed at this point. If YES: check item A1 MREVTYPE. Does MREVTYPE = 2 (In a Hospital Outpatient Department)? If NO, no soft check is displayed at this point. If YES, display a soft check message:
ONE OR MORE CODES/MODIFIERS INDICATES TELEHEALTH, BUT THE LOCATION OF SERVICE SELECTED IS NOT TELEHEALTH. CONFIRM THE CURRENT LOCATION OF SERVICE AND CONTINUE OR CLICK THE GOTO BUTTON TO CHANGE THE LOCATION OF SERVICE TO TELEHEALTH.
2022 UPDATE: Modifiers added in MCPT must be 2 characters. After the first 5 characters in an MCPT field, any additional entry within that same field must be 0 characters or 2 characters.
2020 UPDATE: Values entered into MCPT are checked against a dictionary of valid CPT-4 and HCPCS codes. Entry is allowed for valid codes. If entry of an invalid code is attempted, a hard check message is displayed, “The code you entered is not in our database. Please verify your entry. If the entry is correct, leave MCPT empty and move to MCPTDS field to enter a description instead.”
2016 UPDATE: REQUESTING EVENT FORM CHANGE IN WHAT IS CONSIDERED AN ERROR FOR A6a/b GRID. [The following only occurs during re-abstraction: If an event includes a duplicated CPT code and associated charge that needs to be deleted, the deletion creates errors for all CPTs/charges listed after it, even if their CPTs or values do not change. This happens when the deleted item is not the last in the list/grid. For example, if the second CPT and associated charge in the list is deleted, the system marks that removal as an error. Then it shifts every CPT and charge “below” that one in the grid. Each one of those shifts counts as an error. Requesting Event Form change in what is considered an error.]
Design Note for A6b
Move the gray interviewer NOTE up above the OTHERMCPT variable.
Design Note for C2
C2. [I show the total charges as OUT_TOTLCHRG / I show the payment as undetermined. / I show the payment as OUT_TOTLCHRG, although one or more payments are missing ] Is that correct? IF INCORRECT, CORRECT ENTRIES SHOWN ABOVE AS NEEDED.
CHARGES
Services charge: CPT-4 CODE: [MCPT_1] / DESC: [MCPTDS_1] charge = $[MCPTCH_1]
.
.
.
Services charge: CPT-4 CODE: [MCPT_N] / DESC: [MCPTDS_N] charge = $[MCPTCH_N]
Inpatient charge: Total amount = $[IN_TOTLCHRG]
Programmer:
At least one entry of MCPTCH must be something other than -4. Entries of dollars, DK, RF all count as valid entries in the presence of -4. If a user answers A6_Anymore (“Any more procedures”) as “No” and the sole entry is -4 or all entries are -4, then administer a hard check message: “At least one charge must have a value other than -4.”
If user enters -5 in MCPTCH even once, then all such entries should be -5 or administer a hard check “If charges are linked to another event, then record each charge in this event as -5.”
When a user answers A6_Anymore (“Any more procedures”) as “No”, and one or more MCPTCH entries equals DK, RF administer a soft check message: “One or more charges was recorded as Don’t Know or Refused. Press review and correct if needed, or suppress and continue.”
A6b: 0 is UNALLOWABLE. Must have a positive value, -4, -5, DK or REF response.
IF C2=NO + “NEXT” SEND USER BACK TO FORM A6. [ACCOMPLISHED WITH A HARD CHECK.]
Validation: If OUT_TOTLCHRG>30000 administer soft-check “You have entered a charge over $30,000. Please review and correct if needed, or suppress and continue.”
A6a - [SYSTEM WILL SET UP AS A LOOP, SO NO LIMIT ON CPT-4 CODES REQUIRED]
A6a and A6b is a question loop that will require:
A HISTORY BOX to display responses already collected.
(2) A question to appear after each iteration of the questions that reads: Any More Services? YES=1 NO=2
A6a – (this visit/these visits) – If A5a=YES fill: "these visits" ELSE fill: "this visit".
A6a – For MCPT field, display “CPT-4 Code” and “SUM OF KNOWN CHARGES = “. Sum of known charges displays running total of charges entered for the event.
A6a – For MCPTDS field, display “SUM OF KNOWN CHARGES = “. Sum of known charges displays running total of charges entered for the event.
A6a – Field length allows up to 100 characters.
A6b, IF NO CHARGE – (s) – If A6a has one response fill: “ “ ELSE fill: “s”.
A6b, IF NO CHARGE – (this/these) – If A6a has one response fill “this” ELSE fill: “these”.
A6b, VERIFY – (Is this/Are these) - If A6a has one response fill: "Is this" ELSE fill: "Are these".
A6b, VERIFY – (s) - If A6a has one response fill: " " ELSE fill: "s".
A6b, VERIFY – (this/these) - If A6a has one response fill: "this" ELSE fill: "these".
C2 – customized wording. If there is even one reserve code entered in the charge fields, then end the currently displayed phrase with “…although there are some charges that are missing.” Do not use the word “total” because we don’t know the true total. For example:
“I show the charge as $30, although one or more charges is missing. Is that correct?”
“I show the charge as zero, although one or more charges is missing. Is that correct?”
If all the entries in the SOP fields are reserve codes, then display:
“I show the total charge as undetermined.”
DOLLAR AMOUNTS SHOULD BE FORMATTED TO INCLUDE COMMAS and DECIMAL POINTS
A6a - DK/REF – CONTINUE TO A6b
A6b - DK/REF – CONTINUE TO C2
C2 – A6b = -5 (RESERVE CODE INDICATING CHARGES LINKED TO OTHER EVENT) CONTINUE TO LC2
C2 – A2a <> -5 (NOT LINKED TO ANOTHER EVENT) THEN GO TO C3 FEEORCAP
C2: DK/REF NOT ALLOWED
Do a check that -5 is entered for all MPCT# or none at all. Check that at least 3 characters are entered in MCPTDS#.
[After C2 – continue to C3]
[Page 14 – PATIENT ACCOUNTS - SERVICES/CHARGES – OUTPATIENT/ER/OTHER (2 of 2)]
LC2 You reported just now that the charges are linked to another event. What was the date of that other event where the charges appear?
ENTER A DATE IN THE FORMAT MM/DD/YYYY. INCLUDE LEADING 0’s FOR SINGLE DIGIT MONTHS AND DAYS
LC3 And what kind of event was that, was it… |
OTHMCPT_DATE
Inpatient 1 Hospital Outpatient Department. 2 Hospital Emergency Room 3 Long term care unit such as skilled nursing facility 4 Somewhere else? 5 OTHMREVTYPE OTHMREVTYPETXT
|
PROGRAMMER NOTES
OTHMCPT_DATE -- value for month should be between 1 and 12
OTHMCPT_DATE -- value for day (DD) should only valid numbers (1-28 for all months; 29-30 for all months except month 2; 31 allowed only for months 1, 3, 5, 7, 8, 10, and 12; value 29 allowed for month 2 only in leap years)
OTHMCPT_DATE -- value for year should be 2021, 2022, or 2023. (Add hard check for years other than 2021, 2022, or 2023: “YEAR MUST BE 2022, PLEASE CORRECT”).
LC2 – DK/REF, CONTINUE TO LC3
IF LC3 OTHMREVTYPE = “Somewhere else”, OTHMREVTYPETXT DISPLAYS: “Specify other location”. TEXT FIELD ALLOWS UP TO 30 CHARACTERS.
LC3 –CONTINUE TO LSPCHECK
2021 UPDATE: For linked events (MCPTCH = -5), instrument skips from completed LC3 to LSPCHECK (skipping payment items) because payments are captured in linked event.
EDIT SPECS FROM WESTAT
QA6a PROCEDURES / CHARGES
PROCEDURE IS A CRITICAL ITEM / CHARGE IS NOT A CRITICAL ITEM Follow Skip Pattern
-
DATA ITEM
SPECIFICATIONS
ACTION, if specification not met
QA6a
PROCEDURES
PROCEDURE IS CRITICAL ITEM
Used for Determining SBDs
There must be at least one procedure, written as a text description, or a CPT code or a HCPC.
Blue Sheet, if procedure is missing.
DK and RF are acceptable answers.
Change DK to –8. Change RF to –7. Give an RC code of 60 (critical item missing).
Descriptions of procedures must be clear, valid, and legible.
Blue Sheet.
Descriptions cannot be more than 100 characters.
Ask a team leader to shorten it, or Yellow Sheet.
Abbreviations in the Description field should be standard medical abbreviations.
Review abbreviations.
Check reference list in manual.
Check medical dictionary.
Ask team leader to check website.
Yellow Sheet, if not found, or team leader not available.
CPT and HCPC codes must fall within valid ranges (see Cheat Sheet).
Blue Sheet.
HCPCs cannot begin with W, X, Y, or Z because these are local codes, not national codes.
Blue Sheet, asking for text description.
CPT and HCPC Modifiers must be valid. Valid modifiers include:
2 numbers
2 letters
1 letter + 1 number
1 letter
Keep all valid modifiers.
Cross out all invalid modifiers.
Note: Modifiers with X may be a multiplication sign – see below.
Only one procedure per line.
Procedures cannot be followed by a multiplication mark
(For example: 85025 x5).
Multiplication marks should not be confused with modifiers.
Blue Sheet, saying that there can only be one procedure per line.
Only one valid modifier is acceptable for each CPT code.
Cross out the second modifier.
Modifiers must be separated from the main code by a hyphen.
Change a decimal point to a hyphen.
Multiple visits may need review
Check CPT codes in the 99201–99499 range.
Accept OP codes w/consultation codes.
Accept OP codes w/ preventive medicine codes.
Yellow Sheet multiple OP codes in the same book.
Accept multiple ER codes in the same book.
If it looks like both an ER and an OP event are included in one book, Yellow Sheet.
If it looks like an HS event is combined with an OP or ER event, Yellow Sheet.
Procedures should be consistent with the location of the event (event type).
See PROCEDURE NOTES on pages 5-22 and 5-23.
Compare procedure to QA1.
Yellow Sheet, if not consistent.
PROCEDURES THAT NEED SPECIAL HANDLING
PROCEDURES |
Specification |
Action |
Body part with no procedure |
Body part alone is not a valid procedure. |
Blue Sheet. |
Body part with indication of Radiology |
Body parts with descriptive phrases that indicate Radiology are acceptable. For example, 2 views, P/A, LAT, v |
Accept. |
Abbreviations |
Standard medical abbreviations are allowed. Shorthand abbreviations are not accepted. |
Look up in abbreviations reference book or medical dictionary. Ask a team leader to look up on a website. Yellow Sheet, if a team leader is not available. |
CPT code with description |
Should not have a code and a description on the same line. 71020
|
Look up code. If code and text do not match, Blue Sheet, asking if they are one procedure or two. If the code and text match, cross out text. |
CPT code with units |
Allowed for anesthesia codes and J-code HCPCs. 99284
J2001
|
Keep if anesthesia or J-code. Circle as one answer. Blue Sheet if any other code, saying that there can only be one procedure per line. |
CPT code with multiplication mark |
Not allowed. 71020 (x2) |
Blue Sheet, saying that there can only be one procedure per line. |
State tax |
Valid if it is not the only service in the book. Cannot stand alone. Needs further review. No identifying information is allowed. |
Yellow Sheet, if it is the only procedure.
Cross out state name, if given. |
Handling 99000 - 99002 |
Valid if it is not the only service in the book. Cannot stand alone. Needs further review. |
Yellow Sheet, if it is the only procedure. |
Administrative fee |
Valid if it is not the only service in the book. Cannot stand alone. Needs further review. |
Yellow Sheet, if it is the only procedure. |
Surcharge |
Cannot stand alone. Needs further review. Valid if it is not the only service in the book. No identifying information is allowed. |
Yellow Sheet, if it is the only procedure. Cross out state name, or other identifying information, if given. |
Ambulance, ambulance mileage |
Needs further review. |
Yellow Sheet. |
Reports, copy of reports, insurance reports |
Valid if it is not the only service in a book. |
Yellow Sheet if only procedure. |
99080 S9981, S9982 |
Valid if it is not the only service in a book. |
Yellow Sheet if only procedure. |
Rx pickup; Pharmacy |
Valid if it is not the only service in a book. |
Yellow Sheet if only procedure. |
Canceled appointment, no show charge |
Needs managerial review. |
Yellow Sheet. |
“No Facility Fee” comment |
Needs managerial review. |
Yellow Sheet. |
Follow up, no charge |
We take charge equivalents. |
Blue Sheet. Is this part of the Global Fee? If not, can we get a Charge Equivalent? |
Service with no charge or comment that facility did not charge for a procedure. |
We take charge equivalents. |
Blue Sheet, asking for a Charge Equivalent. |
ER event with OBSERVATION, 99217-99220, 99234-99236 |
Observation is usually OP. |
Blue Sheet to ask if we are missing an OP event. Address blue sheet to TRC SPVR. |
99024 (Follow-up visit included in a Global Fee) |
A Global Fee f/u visit should appear as a GF date in the book with the main GF charge. It should not have a separate book. |
Blue Sheet. Should this be part of a global fee? |
Proc is DK or RF / Charges are DK or RF / Payments are DK or RF. |
If all three are DK or RF, booklet needs managerial review. |
Yellow Sheet. |
99500 – 99600 (Home Care services) |
If there are Home Care services the Patient Data Form must be reviewed. Did we expect Home Care events? |
Accept, if no Home Care Events were reported on Patient Data Form. Blue Sheet if Home Care events were reported, asking that they be collected. |
CPT code indicates inpatient care, but not an HS event. |
Hospital codes are allowable for any hospital event. |
Accept inpatient care with inpatient, outpatient or emergency room event. |
CPT code indicates ER care but not an ER event. |
Hospital codes are allowable for any hospital event. |
Accept emergency room event, inpatient event, or outpatient event. |
CPT code indicates OP or HS event but there is an ER MED SBD. |
ER doctors may be involved in non-ER events. |
Accept ER doctors in events that are not ER.
|
Delivery 59400 – 59412, 59510-59525, 59610 – 59622 |
Valid for HS event. Verification needed for MV, OP, or ER. |
Blue Sheet to verify that event took place in physician’s office or OP dept or ER. |
Neonatal inpatient care 99295 – 99299, 99433, 99436 |
Valid for HS event. Verification needed for MV, OP, or ER. |
Blue Sheet to verify that event took place in physician’s office or OP or ER. |
CHEAT SHEET RANGES FOR PROCEDURES (CPT-4 and HCPC)
[Modifiers are separated by a hyphen – may be 2 numbers or 2 letters, a number and a letter, or one letter.]
CPT4 – 5 DIGITS:
Anesthesiology
00100 to 01999, 99100, 99116, 99135 & 99140
Surgery
10021 - 19499
20000 - 29999
30000 - 39599 (36400 - 36425 are not surgery)
40490 - 49999
50010 - 59899 (59020 & 59025 are not surgeries)
60000 - 69990
93501 - 93545, 93580 - 93581
Radiology
70010 - 79999
938_ _, 939_ _
Pathology and Laboratory
80048 - 89356
36400 - 36425, 36540
also HCPC G0001
Medicine
90281 - 99602 [HH = 99500 – 99602]
Evaluation and Management
99201 - 99499 [ER = 99281 – 99288)
HCPC – ‘ALPHA’ + 4 DIGITS STARTING WITH A, B, C, D, E,G, H, J, K, L, M, P, Q, R, S, T, V
[Do not accept W, X, Y, Z – Blue Sheet for text description]
QC2 TOTAL CHARGE Follow Skip Pattern
-
DATA ITEM
SPECIFICATIONS
ACTION, if specification not met
QC2 - Total Charge
Total Charge must be written by the TRC.
Blue Sheet.
Total Charge should equal sum of Individual Charges.
If there is only one charge, compare to Total. Blue Sheet if not the same.
Calculator tape should be run to verify Total if there are multiple charges.
Do not use the TRC’s tape.
Run calculator tape.
If tape doesn’t match book, write NOT OK.
If tape matches book, write OK.
Initial the tape.
If the Total Charge written by the TRC is less than sum of the Individual Charges, a correction can be made if the difference is 10% or less.
Compare the amount of the difference and the Total Charge as written by the TRC.
Note that changes can affect the answers to Box 2 and QC6.
If the difference is 10% or less than the Total, correct the Total Charge.
Blue Sheet, if the difference is greater than 10%.
Change Box 2 to the appropriate answer.
Blue Sheet, if QC6 was skipped, but now must be answered.
If the Total Charge written by the TRC is greater than the sum of the Individual Charges, the TRC must make any corrections.
Blue Sheet.
DK or RF is acceptable.
If Total Charge, and Total Pay, and Procedures are all DK or RF, Yellow Sheet.
If one charge is DK or RF, Total Charge should be DK or RF.
Yellow Sheet.
$0.00 is not acceptable. Nothing is Free.
Yellow Sheet.

SECTION 11 – PATIENT ACCOUNTS – SERVICES/CHARGES – INPATIENT/LTC
NOTE: See end of section for edit specs from Westat for questions A8, A9, A10a, and C2a.
[Page 15 – PATIENT ACCOUNTS - SERVICES/CHARGES – INPATIENT/LTC (1 of 6)]
SCREEN LAYOUT
A8. According to Medical Records, (PATIENT NAME) was (in long term care / an inpatient) during the period from [ADMIT DATE] to [DISCHARGE DATE]. What was the DRG for this stay?
DRG IS A CODE USED TO CLASSIFY INPATIENT STAYS AND IT IS USUALLY ONE TO THREE DIGITS LONG.
IF NO DRG, ENTER F6 (DON’T KNOW).
|
DRG: STAYDRG
DRG NOT RECORDED:……………………….1 NODRG |
PROGRAMMER NOTES
The check for an entry in either STAYDRG or NODRG should be a hard check, with message “Enter a DRG or put ‘1’ in the NODRG field if none recorded for this event.”
[If STAYDRG GO TO C2a.
If NODRG GO TO A9.]
SYSTEM WILL COLLECT A RANGE OF 1 TO 989 FOR THE DRG.
(PATIENT NAME) should fill with patient’s first name and patient’s last name from Housing Component data file.
[ADMIT DATE] should fill with INPATBEG_DAT from A2a.
[DISCHARGE DATE] should fill with INPATEND_DAT from A2a.
DK/REF – CONTINUE TO A9.
2019 UPDATE: Add fill of “in long term care” or “an inpatient” depending on the response to item A1. If response = 1, use “an inpatient” as fill. If response = 5, use “in long term care” as fill.
2019 UPDATE: If STAYDRG is DK or REF, go to NODRG.
[Page 16 – PATIENT ACCOUNTS - SERVICES/CHARGES – INPATIENT/LTC (2 of 6)]
SCREEN LAYOUT
A9. Did the patient have any surgical procedures during this stay? |
YES=1, NO=2 ANYSURG
|
PROGRAMMER NOTES
[If ANYSURG = 2 GO TO C2a.]
A9 - DK/REF – GO TO C2a
[Page 17 – PATIENT ACCOUNTS - SERVICES/CHARGES – INPATIENT/LTC (3 of 6)]
SCREEN LAYOUT
A10a. What surgical procedures were performed during this stay? Please give me the procedure codes, that is the CPT-4 codes, if they are available. IF CPT-4 CODES ARE NOT USED, DESCRIBE SERVICES AND PROCEDURES PROVIDED. ENTER UP TO 8 CHARACTERS. IF CODE BEGINS WITH W, X, Y OR Z, ENTER A DESCRIPTION INSTEAD. IT IS ACCEPTABLE TO ENTER ICD-10-PCS CODES IN THE DESCRIPTION FIELD FOR THIS QUESTION IF A PROCEDURE CODE OR DESCRIPTION IS NOT AVAILABLE. |
CODE DESCRIPTION SRGCPT# SRGDES#
SRGCPT# SRGDES#
SRGCPT# SRGDES#
SRGCPT# SRGDES#
|
PROGRAMMER NOTES
A10a - [SYSTEM WILL SET UP AS A LOOP, SO NO LIMIT ON CPT-4 CODES REQUIRED]
A10a is a question loop that will require:
A HISTORY BOX to display responses already collected.
( 2) A question to appear after each iteration of the questions that reads: Any more surgical procedures? YES=1 NO=2
A10a - DK/REF – CONTINUE TO C2a
SRGDES field allows up to 100 characters.
[Page 18 – PATIENT ACCOUNTS - SERVICES/CHARGES – INPATIENT/LTC (4 of 6)]
SCREEN LAYOUT
C2a. What was the full established charge for this (long term care / inpatient) stay, before any adjustments or discounts?
[IF ADFROMER=1] Please do not include any emergency room charges, unless they cannot be separated from the [inpatient/long term care] charges.
EXPLAIN IF NECESSARY: The full established charge is the charge maintained in the hospital’s master fee schedule for billing insurance carriers and Medicare or Medicaid. It is the “list price” for the service, before consideration of any discounts or adjustments resulting from contractual arrangements or agreements with insurance plans.
IF NO CHARGE: Some facilities that don’t charge for each individual service do associate dollar amounts with services for purposes of budgeting or cost analysis. This is sometimes called a “charge equivalent.” Could you give me the charge equivalent for this inpatient stay?
NOTE: WE NEVER ENTER $0 FOR A CHARGE
|
FULL ESTABLISHED CHARGE OR CHARGE EQUIVALENT:
$IN_TOTLCHRG
|
[Page 19 – PATIENT ACCOUNTS - SERVICES/CHARGES – INPATIENT/LTC (5 of 6)]
C2b [IF ADFROMER=1] Were the emergency room charges included with the full established charge? |
YES=1, NO=2 ERCHRINC |
C2b - DK/REF AND MREVTYPE= 5 CONTINUE, OTHERWISE SKIP TO C3
[Page 20 – PATIENT ACCOUNTS - SERVICES/CHARGES – INPATIENT/LTC (6 of 6)]
C2c [IF MREVTYPE (A1) = 5] Were the ancillary charges included with the full established charge? |
YES=1, NO=2 ANCILL |
C2c: DK/REF GO TO C3
PROGRAMMER NOTES
IF C2a = DK/REF administer a soft check that states the following “The charge was recorded as Don’t Know or Refused. Please review and correct if needed, or suppress and continue.”
0 is UNALLOWABLE. Must have a positive value or DK/REF response
Validation: If IN_TOTLCHRG>250,000 administer soft-check “You have entered a charge over $250,000. Please review and correct if needed, or suppress and continue.”
ONLY DISPLAY TEXT READING “Please do not include any emergency room charges, unless they cannot be separated from the [inpatient/long term care] charges.” IF ADFROMER (from A2b) =1.
Fill [inpatient/long term care]: If MREVTYPE = 1, fill “inpatient”; if MREVTYPE = 5, fill “long term care”.
ONLY DISPLAY TEXT READING “Were the emergency room charges included with the full established charge?” IF ADFROMER (from A2b) =1. For ERCHRINC: If ADFROMER (from A2b)=2 code ERCHRINC=2
ONLY DISPLAY TEXT READING “Were the ancillary charges included with the full established charge?” IF MREVTYPE (from A1) = 5.
VERIFY – (this/these) - If A8 or A10a has one response fill: "this" ELSE fill: "these".
VERIFY – (s) - If A8 or A10a has one response fill: " " ELSE fill: "s".
DK/REF – CONTINUE TO C3
2019 UPDATE: Add fill of “in long term care” or “an inpatient” depending on the response to item A1. If response = 1, use “an inpatient” as fill. If response = 5, use “in long term care” as fill.
[After C2a, CONTINUE TO C3]
EDIT SPECS FROM WESTAT
QA8 – QA10b INPATIENT SERVICES
DRG or Surgery Procedures is a Critical Item Follow Skip Pattern
DATA ITEM |
SPECIFICATIONS |
ACTION, if specification not met |
QA8 - DRG or NOT
CRITICAL ITEM
USED FOR DETERMINING if we need SBDs for SAP |
A DRG must be given or 1 (DRG NOT RECORDED) |
Blue Sheet, if no DRG is given and 1 is not circled. |
DK or RF is acceptable, but need managerial review. |
Yellow Sheet. |
|
DRG must be within valid range. 1 to 989 for inpatient stays 996 for IC events only |
Check Cheat Sheet. Blue Sheet, if not a valid range. |
|
DRG must be determined to be surgery or non-surgery. |
Check Cheat Sheet. If DRG indicates surgery, ask for SAP. If DRG indicates non-surgery service, put Ø on front cover of book and do not ask for any SBDs. |
|
QA9 – Surgery or not
USED FOR DETERMINING if we need SBDs for SAP
|
This question is skipped if a DRG is given. |
Cross out the answer to QA9 if DRG is given in QA8. |
YES (1) or NO (2) must be circled if no DRG is given (YES or NO must be answered in QA9, if QA8 is 1 – NO DRG RECORDED.) |
Blue Sheet, if response is missing and the TRC has not indicated DK or RF. |
|
DK or RF needs managerial review. |
Yellow Sheet. |
|
Answer must be compared to data on SBD forms. |
Check SBD forms for indication that surgery was done. If there are SBDs for SAPs, and QA9 is NO surgery, Blue Sheet asking if a surgery procedure was performed. |
|
Answer must be YES if there are surgical procedures in QA10a. |
Change to YES, if there are surgical procedures listed in QA10a. If unsure that procedures are surgeries, ask a team leader or Yellow Sheet. |
|
For inpatient stays the only specialties to be accounted for are SAPs. If there is no surgery, we do not ask for any specific specialty, although we accept all Separately Billing Doctor SBD forms. |
If YES, surgery performed, ask for SAP. If NO surgery, put Ø on front cover of book and do not ask for any SBDs. Accept any SBD forms that are Separately Billing. If there are no SBD forms for this event, review QA3. |
|
QA10a – SURGICAL PROCEDURES
CRITICAL ITEM
|
QA10a should be skipped if QA8 is answered. |
Yellow Sheet, if a DRG is given in QA8 and surgical procedures are given in QA10a. |
CPT codes are acceptable. CPT codes must be valid and have valid modifiers. |
Check Cheat Sheet. See page 5-21 for CPT procedure spex. Blue Sheet, if procedure code is not valid. |
|
Text descriptions must be clear, legible and valid as surgeries. |
Blue Sheet. |
|
Any abbreviations must be standard medical abbreviations. |
Review abbreviations. Check reference list in manual. Check medical dictionary. Ask team leader to check website. Yellow Sheet, if not found, or team leader not available. |
|
Text descriptions must be 100 characters or less. |
Yellow Sheet or ask a team leader to shorten it. |
|
Two-digit ICD-10 procedure codes are acceptable. For example, 44.41. 01 – 99.99 |
Blue Sheet, if not valid. |
|
Surgical Procedure Counter. |
Office Use Only box must be filled in. |
Count the number of surgery procedures and enter as a 2-digit, zero-filled number. |
Procedure of DK or RF = Procedure count of 01. |
||
Only one diagnosis may be checked as the Principal Procedure. |
If more than one procedure is checked, cross out the checkmarks and circle –8, Principal Procedure is not known. |
|
A Principal Procedure should not be identified if there is only one procedure. |
Cross out the checkmark if there is only one procedure. |
QC2 a-b INPATIENT CHARGES Follow Skip Pattern
DATA ITEM |
SPECIFICATIONS |
ACTION, if specification not met |
QC2 a – Inpatient Charges
|
Must be answered.
|
Blue Sheet, if blank. Yellow Sheet, if blank, but there is a comment explaining why. |
DK and RF answers are acceptable. |
Accept. Change DK to – 8. Change RF to –7. Since charges are not critical items, the Receipt code will not change from 63 to 60 based on this question. |
|
Acceptable Range > or = $1000.00, except newborn Acceptable Range > or = $500.00 for newborn. |
Yellow Sheet, if less than $1000, unless newborn. Yellow Sheet, if newborn and less than $500.00 |
|
$0.00 charge is not acceptable. N/C is not acceptable. “NO CHARGE” is not acceptable. |
Yellow Sheet.
|
|
Managerial Review is needed if Charges, Procedures, and Payments are all DK or RF. |
Yellow Sheet. |
|
QC2b
FOR HS event: ER charges included or not FOR IC event: Ancillary charges included or not |
FOR HS QC2b: YES (1) or NO (2) must be answered. |
Blue Sheet if blank. |
If YES (1) circled, QA2b and BOX 4 must be ADMITTED FROM ER (1). |
Blue Sheet
|
|
If YES, there must be an ER booklet. |
Blue Sheet, if there is no ER booklet. |
|
If YES, this indicates a link. |
GO TO LINK SECTION, page 5-24. Blue Sheet, if ER book is not written as a link. |
|
Linked books must be in 2022. GO TO LINK SECTION, page 5-24. See also CHECKLIST FOR 2022 OR 2023 LINKED BOOKS. |
If an ER book was deleted, leave QC2b as “1,” ER charges included. Write a comment stating that book was deleted. Initial comment. |
|
FOR IC QC2b: 1 or 2 circled. (Institution cases will be done by specially-trained editors.) |
Fix the answer by using the Ancillary section of the Institution event booklet. |
SECTION 12 – PATIENT ACCOUNTS – REIMBURSEMENT TYPE
[Page 21 – PATIENT ACCOUNTS - REIMBURSEMENT TYPE (1 of 1)]
SCREEN LAYOUT
C3. Was the facility reimbursed for (this visit/these visits/this stay) on a fee-for-service basis or capitated basis?
EXPLAIN IF NECESSARY: Fee-for-service means that the facility was reimbursed on the basis of the services provided.
Capitated basis means that the patient was enrolled in a prepaid managed care plan where reimbursement is not tied to specific visits, this is also called Per Member Per Month.
IF IN DOUBT, CODE FEE-FOR-SERVICE.
|
Fee-for-service basis =1 FEEORCAP Capitated basis =2
|
PROGRAMMER NOTES
IF FEEORCAP=2 GO TO C7a
(this visit/these visits/this stay) – If MREVTYPE (A1) = 2, 3, or 4 and GLOFEE (A5a) =YES fill: "these visits". If MREVTYPE (A1) = 2, 3, or 4 and GLOFEE (A5a) =NO fill: "this visit". If MREVTYPE = 1 or 5 fill: “this stay”.
DK/REF – CONTINUE TO C4
EDIT SPECS FROM WESTAT
QC3 REIMBURSEMENT TYPE Follow Skip Pattern
-
DATA ITEM
SPECIFICATIONS
ACTION, if specification not met
QC3 Fee for Service or Capitated?
CRITICAL ITEM
1 or 2 must be circled.
This critical item can usually be determined by looking at the skip pattern of the payment questions.
If blank, answer 1 or 2, by looking at the skip pattern used for the payment questions.
Answer must be consistent with the skip pattern used in payments section.
If Fee for Service, then QC4, Box 1, and QC6 must be answered.
If Capitated, then QC7a – f Capitated Section must be answered.
If answered incorrectly, circle the answer that matches the skip pattern, and cross out incorrect response.
Should be consistent in all books for a patient, unless there is an explanation.
Yellow Sheet, if there is no explanation about a change in insurance which caused the change among books.
SECTION 13 – PATIENT ACCOUNTS – SOURCES OF PAYMENT
[Page 22 – PATIENT ACCOUNTS - SOURCES OF PAYMENT (1 of 1)]
SCREEN LAYOUT
C4. From which of the following sources has the facility received payment for (this visit/these visits/this stay) and how much was paid by each source? Please include all payments that have taken place between (DATE) and now for (this visit/these visits).
IF NONE, ENTER ZERO (0).
[DCS ONLY] IF NAME OF INSURER, PUBLIC, OR HMO, PROBE: And is that Medicare, Medicaid, or private insurance?
[DCS ONLY] IF PROVIDER VOLUNTEERS THAT PATIENT PAYS A MONTHLY PREMIUM, VERIFY: So, you receive a monthly payment rather than payment for the specific service? IF YES: GO BACK TO C3 AND CODE AS CAPITATED BASIS.
|
SOURCE
a. Patient or Patient’s Family;
b. Medicare;
c. Medicaid;
d. Private Insurance;
e. VA/ChampVA;
f. Tricare;
g. Worker’s Comp; or
h. Something else? (IF SOMETHING ELSE: What was that?) OTPAYMOS OTPAYMOSTXT
|
PAYMENT AMOUNT $PATPAYM
$CAREPAYM
$AIDPAYM
$PINSPAYM
$VAPAYM
$CHAMPAYM
$WORKPAYM
$OTHRPAYM |
C5. [I show the total payment as TOTPAYM / I show the payment as undetermined. / I show the payment as TOTPAYM, although one or more payments are missing ] Is that correct? / [THE TOTAL PAYMENT IS TOTPAYM . IS THAT CORRECT?
IF NO, CORRECT ENTRIES ABOVE AS NEEDED.
|
TOTAL PAYMENTS
|
$ TOTLPAYM |
PROGRAMMER NOTES
When a user answers MoreSources_1 (“Any more payments”) as “No”, and one or more entries among PATPAYM, CAREPAYM, AIDPAYM, PINSPAYM, VAPAYM, CHAMPAYM, WORKPAYM equals DK, RF administer a soft check message: “One or more payments was recorded as Don’t Know or Refused. Please review and correct if needed, or suppress and continue.”
2019 UPDATE: Each C4 item a-h (PATPAYM to OTHERPAYM) appears on its own screen, along with the entire C4 question text and DCS instructions. Each screen has the word “SOURCE:” before the source (Medicare, Private Insurance, etc.) being asked about on a given screen. The differences among screens is only the source being asked about.
Require an entry in each source of payment (SOP) field PATPAYM to WORKPAYM. Require an entry in OTHRPAYM if MoreSources = 1. The following are allowed entries: 0, integer, integer with 2 decimal places, F6/DK, F7/REF.
In the summary of charges that displays, “I show the total payment as [TOTLPAYM]” distinguish different types of reserve codes, by displaying phrases “Don’t Know” or “Refused” instead of the generic word “missing.”
If there is even one reserve code entered in the SOP fields, then end the currently displayed phrase with “…although one or more payments are missing.” Do not cite “total.” For example:
“I show the payment as $30, although one or more payments is missing. Is that correct?”
“I show the payment as zero, although one or more payments is missing. Is that correct?”
If all the entries in the SOP fields are reserve codes, then display:
“I show the total payment as undetermined.”
TOTLPAYM counts entries of DK or REF in the individual SOPs as “0”.
This variable that is recorded on screen C5 is called TOTLPAYMOK, it saves values of Yes or No. It is a critical item.
FILL INSTRUCTIONS:
All SOP >=0 (e.g., 0, integer dollars, dollars + cents)
Text: I show the total payment as TOTLPAYM.
All SOP <0 (e.g., hotkeys F6 and F7 whose numeric values are -1 and -2)
Text: I show the total payment as undetermined.
Mixed entries (e.g., a zero or dollar amount along with one or more DK/REF)
Text: I show the payment as TOTLPAYM, although one or more payments are missing.
Even if all the individual payments recorded in C4 are DK or REF and the value of TOTLPAYM=0, then we collect either
Reasons for payment < > charges (e.g., PLC1 and the appropriate screens for C6)
Confirmation that payment = charge (C5a).
If a particular SOP was coded as “Don’t Know” or “Refused” then display the appropriate phrase instead of the generic word “missing.”
(VISIT DATE) should fill with OUTPAT_DATE from A2c if MREVTYPE = 2, 3, or 4. (VISIT DATE) should fill with INPATBEG_DAT if MREVTYPE = 1 or 5 and ADFROMER = 2. (VISIT DATE) should fill with OUTPAT_DATE if MREVTYPE = 1 or 5 and AFROMER = 1.
C4 - [SYSTEM WILL SET UP “SOMETHING ELSE” AS A LOOP, SO NO LIMIT REQUIRED]
C4 – (this visit/these visits) - If B2a=YES fill: "these visits" ELSE fill: "this visit".
C4h - The OTPAYMOSTXT variable was added to record free-form text for the “Other, Specify” option. Interviewers will be able to record responses in the text box that do not occur in the listed options Field = up to 50 characters.
C4h is a question loop that will require:
A HISTORY BOX to display responses already collected.
A question to appear after each iteration of the question that reads: Any more sources? YES=1 NO=2
The “something else” option should be set up so a response can be selected from among response options, or entered in as text.
C4h – Include the following options for the “Other Specify”;
Auto or Accident Insurance
Indian Health Service
State Public Mental Plan
State/County/Local program
Other
C5 – System should compute and display total payments from preceding charges reported in fields $PATPAYM# through $OTHRPAYM. The dollars total is referred to in spec as $TOTLPAYMand will be a fill in the C5 question. The answer for the user is Yes or No. However if the user answers “No” then a hard check error message should be administered, “IF INCORRECT, CORRECT ENTRIES AS NEEDED” and return user to previous screen.
C4 - DK/REF – CONTINUE TO C5
C5 - DK/REF – CONTINUE TO BOX 1
DOLLAR AMOUNTS SHOULD BE FORMATTED TO INCLUDE COMMAS and DECIMAL POINTS
Design Note for C5
C5.
CHARGES
Services charge: CPT-4 CODE: [MCPT_1] / DESC: [MCPTDS_1] charge = $[MCPTCH_1]
.
.
.
Services charge: CPT-4 CODE: [MCPT_N] / DESC: [MCPTDS_N] charge = $[MCPTCH_N]
PAYMENTS
Patient or family $[PATPAYM]
Medicare $[CAREPAYM]
Medicaid $[AIDPAYM]
Private insurance $[PINSPAYM]
ChampVA/VA $[VAPAYM]
TRICARE $[CHAMPAYM]
Workers comp $[WORKPAYM]
Other $[OTHRPAYM_1]
Other $[OTHRPAYM_2]
.
.
.
Other $[OTHRPAYM_N]
[I show the total payment as TOTPAYM / I show the payment as undetermined. / I show the payment as TOTPAYM, although one or more payments are missing ] Is that correct?
EDIT
SPECS FROM WESTAT
Decision Log for QC4
PROGRAMMER NOTES Include all “Problems” in a drop down menu at the other specify entry and program the required “decision” behind the scenes. May require implementing instructional boxes for the DCS/abstractor. For example, if the DCS selects “vocational rehabilitation” an instruction box should pop up asking the DCS to probe for source of funding: federal, state, county, other gov’t, private, etc.]
Problem |
Decision / Categorization |
Source of Payments |
|
State (or Federal, or County, or City) Plan ---- Plan may be Fund, Program, Grant ------ type of plan may be given ------- REMOVE Name of State if it is present |
Code by indicating source
of funds, then type of plan if given |
Examples: |
|
Nevada State Disability (SRS) |
Code in 'Other' as State Disability |
State Breast Cancer Program |
Code in 'Other' as State Breast Cancer Program |
Maryland Indigent Program |
Code in 'Other' as State Indigent Program |
Federal Grant |
Code in 'Other' as Federal Grant |
Cook County Indigent Fund |
Code in 'Other' as County Indigent Fund |
State Program |
Code in 'Other' as State Program |
Comment indicates one of the above, but it is not indicated in QC4 (line h) |
Yellow Sheet |
Comment indicates the name of an insurance company for QC4. |
Ignore the name of an insurance company if we have the type of insurance payer. |
QC4 (line h) 'Specify' answer is name of an insurance company |
Blue Sheet to determine source of funding: Federal, State, County, Other gov't, Private etc |
Children's Special Services |
Blue Sheet to determine source of funding: Federal, State, County, Other gov't, Private etc |
Vocational Rehabilitation |
Blue Sheet to determine source of funding: Federal, State, County, Other gov't, Private etc |
Welfare |
Blue Sheet to determine source of funding: Federal, State, County, Other gov't, Private etc |
Hospital Fund |
Blue Sheet to determine source of funding: Federal, State, County, Other gov't, Private etc |
Grant |
Blue Sheet to determine source of funding: Federal, State, County, Other gov't, Private etc |
Grant - DK who is funding it |
Code in 'Other' as GRANT - DK FUNDING |
Breast Cancer Program |
Blue Sheet to determine source of funding: Federal, State, County, Other gov't, Private etc |
Indigent Program or Fund for Indigents |
Blue Sheet to determine source of funding: Federal, State, County, Other gov't, Private etc |
Local |
Blue Sheet to determine who is funding it , I.e. State, County, City, Other gov't, etc |
MediCal (in California) |
Code as Medicaid (C4c) |
Employer |
Yellow Sheet |
Verbiage about car/auto accident paid or auto/car insurance paid |
Code in Other as Auto Insurance |
Military |
Blue Sheet for more specific information |
Indian Health |
Code in Other as Indian Health Service |
CHDP; CHIP |
Accept, but cross out any state or county name |
WIC |
Accept, but cross out any state or county name |
AARP (American Association of Retired Persons) |
Code as Private Insurance (QC4d) |
Prepaid Mental Health Plan - State Plan |
Code In Other as State Public Mental |
HMO |
Blue Sheet to find out Insurance Type: Medicare, Medicaid, Priv Ins., Other; Ask for source of payment. |
BOX 2 DO TOTAL PAYMENTS EQUAL TOTAL CHARGES?
If totChrgFlag = 1 and totPayFlag = 1 (This means no reserve codes were used for any charge and payment variables)
YES, AND ALL PAID BY PATIENT OR PATIENT’S FAMILY -1 (GO TO LSPCHECK)
YES, OTHER PAYERS - 2 (GO TO C5a)
NO, PAYMENTS < CHARGES - 3 (GO TO PLC1)
NO, PAYMENTS > CHARGES - 4 (GO TO ADJEXTRA)
|
IF totChrgFlag =2 AND totPayFlag =2 (This means only reserve codes were used for charge and payment variables – no values recorded) –
-GO TO PLC1 (payments less than charges discrepancy questions)
IF totChrgFlag =2 AND totPayFlag =3 (This means only reserve codes were used for charges and a mix of values and reserve codes was used for payment variables)
- GO TO PLC1 (payments less than charges discrepancy questions)
IF totChrgFlag =3 AND totPayFlag =2 (This means a mix of values and reserve codes were used for charges and only reserve codes were used for payment variables)
- GO TO PLC1 (payments less than charges discrepancy questions)
IF totChrgFlag =3 AND totPayFlag =3 (This means there is a mix of values and reserve codes for charge and payment variables)
- GO TO PLC1 (payments less than charges discrepancy questions)
IF totChrgFlag =1 AND totPayFlag =2 OR totPayFlag =3, AND TOTLPAYM < TOTLCHRG (This means, if we have all the charges, but the payments are either all reserve codes, or have at least 1 reserve code, and the total payment is less than the total charge)
- GO TO PLC1 (payments less than charges discrepancy questions)
IF totChrgFlag =1 AND totPayFlag =3, AND TOTLPAYM > TOTLCHRG (This means, if we have all the charges, and the payments have at least 1 reserve code, BUT the total payment is MORE than the total charge)
GO TO ADJEXTRA (payments more than charges discrepancy question)
[PROGRAM BEHIND THE SCENES – SHOULD NOT APPEAR ON SCREEN. VARIABLE NAME=CPAYBOX]
PROGRAMMER NOTES
DESCRIPTION OF PROGRAMMING REQUIRED FOR BOX 2
IF MREVTYPE=2,3, OR 4 AND
IF C2=C5 AND ONLY C4 OPTION WITH A RESPONSE IS ‘a’ (patient or patient’s family – PATPAYM, GO TO BOX 3.
IF C2=C5 AND C4 OPTIONS b, c, d, e, f, g, or h HAVE A RESPONSE, GO TO C5a.
IF C2≠C5, GO TO C6.
IF C2 OR C5 = DK/REF, GO TO BOX 3
IF MREVTYPE=1 OR 5 AND
IF C2a=C5 AND ONLY C4 OPTION WITH A RESPONSE IS ‘a’ (patient or patient’s family - PATPAYM), GO TO FINISH SCREEN
IF C2a=C5 AND C4 OPTIONS b, c, d, e, f, g, or h HAVE A RESPONSE, GO TO C5a.
IF C2a≠C5, GO TO C6.
IF C2a OR C5 = DK/REF, GO TO FINISH SCREEN.
EDIT SPECS FROM WESTAT
BOX 2 DO PAYMENTS = CHARGES? Follow Skip Pattern
-
DATA ITEM
SPECIFICATIONS
ACTION, if specification not met
BOX 2 – Total Payments = Total
Charges or not
1 (YES), 2 (YES) or 3 (NO) must be circled.
Compare Total Charge to Total Payments.
DK or RF is not acceptable.
Circle 3 (NO).
Blue Sheet for answer to QC6, if skipped.
If 1 (YES) or 2 (YES) is circled, there should be equal dollar values greater than $0.00.
If Total Charge and Total Payments are $0.00, DK or RF, they are not equal. QC6 must be answered.
If Total Charges and Total Payments are $0.00, Yellow Sheet for Total Charges = $0.00.
Change DK or RF to 3 (NO).
Answer QC6 as – 8 (DK).
Cannot be blank.
If blank, circle the correct answer.
Compare Total Payments to Total Charges.
Look at the Source of Payments.
Should be consistent with Total Charges, Total Payments, and Source of Payments.
If answered 1 and it should be 2 or 3, change to the correct answer.
If answered 3, and should be 1 or 2, change to the correct answer.
An answer changed to 2 will follow the skip pattern to QC5a. If that is blank, write a Blue Sheet.
The skip pattern to QC5a cannot be lost.
QC5a is flagged to record the number of times it is answered.
QC5a sends the DCS back to QC4 to look at the payments again. Changes to QC4 will NOT generate a change in Box 2.
Do NOT change the answer 2 (YES) to another answer, even if it is now no longer consistent with QC4 or QC5.
Comments may need special review.
Yellow Sheet.
FOLLOW THE SKIP PATTERN
SECTION 14 – PATIENT ACCOUNTS – VERIFICATION OF PAYMENT
[Page 23 – PATIENT ACCOUNTS - VERIFICATION OF PAYMENT (1 of 1)]
SCREEN LAYOUT
C5a. I recorded that the payment(s) you received equal
the charge(s). I would like to make sure that I have
this recorded correctly. I recorded that the total
payment is [SYSTEM WILL DISPLAY TOTAL
PAYMENT FROM C5]. Does this total payment
include any other amounts such as adjustments or
discounts, or is this the final payment?
IF NECESSARY, READ BACK AMOUNT(S) RECORDED IN C4.
YES, FINAL PAYMENTS RECORDED IN C4 AND C5 =1 EQPAYOK
NO =2
PROGRAMMER NOTES
[IF EQPAYOK=1 and MREVTYPE=2,3, OR 4 GO TO BOX 3.
IF EQPAYOK=1 and MREVTYPE=1 OR 5 GO TO FINISH SCREEN.
IF EQPAYOK=2 DISPLAY HARD CHECK: “IF INCORRECT, RETURN TO C4 AND CORRECT PAYMENT ENTRIES AS NEEDED.”]
payment(s) - If C4 has one response fill: " " ELSE fill: "s".
charge(s) – If MREVTYPE=2,3,or 4 and MCPTCH# (A6b) has two or more responses fill: "s" ELSE fill: " ". If MREVTYPE=1 or 5 fill “ “.
AMOUNT(S) – If C4 has one response fill: “ “ ELSE fill: “s”.
DK/REF – CODE AS 2 (NO) FIRST TIME THROUGH (GOES BACK TO C4), IF NOTHING CHANGES AND END UP BACK AT C5a, GO TO BOX 3 IF MREVTYPE=2,3, OR 4. IF MREVTYPE=1 OR 5, GO TO FINISH SCREEN.
EDIT SPECS FROM WESTAT
BOX 2 and QC5a DO PAYMENTS = CHARGES? Follow Skip Pattern
-
DATA ITEM
SPECIFICATIONS
ACTION, if specification not met
QC5a Verification of 100% payments by Other sources.
QC5a asks the DCS to verify a 100% Total Payment when at least one source of the payment is an insurance program other than the patient.
The skip pattern of Box 2 jumps over this question, unless Box 2 is answered 2.
If QC5a is blank, and Box 2 is 2 (YES, other payer), Blue Sheet for an answer to QC5a.
If QC5a is answered, and Box 2 is answered 1 or 3, cross out the answer.
SECTION 15 – PAYMENTS LESS THAN CHARGES (new section, UNDERPAYMENT)
[Page 24 – SOURCES OF PAYMENT (1 of 1)]
PLC1. It appears that the total payments were less than the total charge. Is that because …
IF THE ONLY PAYMENT FOR THIS EVENT WAS A LUMP SUM, ANSWER “NO” TO ALL OPTIONS.
a. There were adjustments or discounts YES=1 NO=2 DISADJ
b. You are expecting additional payment YES=1 NO=2 MOREPAY
c. This was charity care or sliding scale YES=1 NO=2 SLIDSCA2
d. This was bad debt YES=1 NO=2 BADDEB2
e. Person is an eligible veteran YES=1 NO=2 ELIGVET2
PROGRAMMER NOTES:
2020 UPDATE: If MOREPAY = 1 and BADDEB2 = 1, display a soft check after BADEB2 that reads: “YOU HAVE INDICATED EXPECTING ADDITIONAL PAYMENT AND BAD DEBT AS REASONS PAYMENTS ARE LESS THAN CHARGES. PLEASE CONFIRM WITH THE POC BY ASKING: “If the patient or other payer were to try to make a payment on this bill, would you be able to accept it?” IF YES = Expecting Additional Payment from Patient. IF NO = Bad Debt. IF POC INDICATES BOTH ARE YES, SUPPRESS AND CONTINUE.”
2016 UPDATE:
Create a new Section with single form called UNDERPAYMENT to contain DISADJ, MOREPAY, SLIDSCA2, BADDEB2, and ELIGVET2 spec’d above as PLC1a-d.
ELIGVET2 – allow DK/REF
If MOREPAY=1 then show C6_additional.
If [DISADJ=1 and MOREPAY=1 ] or [DISADJ=2 and MOREPAY=2 and SLIDSCA2=2 and BADDEB2=2] then show C6_additional.
If both SLIDSCA2=1 and BADDEB2=1 with no other selection, do not show C6_additional.
If both SLIDSCA2=1 or BADDEB2=1 with no other selection, do not show C6_additional.
2019 UPDATE: Each PLC1 item a-e (DISADJ to ELIGVET2) appears on its own screen, along with the entire PLC1 question text. The differences among screens is only the reason payments are less than charges being asked about.
ELIGVET2: Display onscreen instruction: “DCS: IF THE POC IS CONFUSED BY THE QUESTION, ANSWER THE QUESTION ‘NO’.”
SECTION 16 – PATIENT ACCOUNTS – DIFFERENCE BETWEEN PAYMENTS AND CHARGES
[Page 25– PATIENT ACCOUNTS - DIFFERENCE BETWEEN PAYMENTS AND CHARGES (1 of 1)]
SCREEN LAYOUT
.
Are you expecting additional payment from:
ADJEXTRA It appears that the total payments were more than the total charges. Is that correct? DCS: IF THE ANSWER IS “NO” PLEASE GO BACK TO C5 (VERIFY TOTAL PAYMENTS) TO RECONFIRM CHARGES AND PAYMENTS AS NEEDED.
YES=1, NO=2
. |
C6_Additional, Question C6_additional Expecting additional payment i. Patient or Patient’s Family? YES=1, NO=2 EPAYPAT j. Medicare? YES=1, NO=2 EPAYCAR k. Medicaid? YES=1, NO=2 EPAYAID l. Private Insurance? YES=1, NO=2 EPAYPINS m. VA/ChampVA? YES=1, NO=2 EPAYVA n. Tricare? YES=1, NO=2 EPAYCHAM o. Worker’s Comp? YES=1, NO=2 EPAYWORK p. Something else? YES=1, NO=2 EPAYOTH (IF SOMETHING ELSE: What was that?) EPAYOTOS EPAYOTOSTXT
|
PROGRAMMER NOTES
2016 UPDATE:
At least one entry among the variables on screen C6_additonal must be a “1”, DK or RF. If all entries in the series are “2” (No) then administer a hard check when the user presses “Next” at C6_Additional, “You must select at least one reason for underpayment.”
At C6_Additional
If Additional pymt expected (MOREPAY) selected as a reason at PLC1, require a selection (1,DK,RF) at C6_Additional. If all are 2, administer a hardcheck. If Sliding Scale and Bad Debt options are shown, include them in the check, otherwise, exclude them.
if ( [MOREPAY] =="1" && [EPAYPAT] =="2" && [EPAYCAR] =="2" && [EPAYAID] =="2" && [EPAYPINS] =="2" && [EPAYVA] =="2" && [EPAYCHAM] =="2"
&& [EPAYWORK] =="2" && [EPAYOTH] =="2" && ([SHOW_SLIDSCA] == "No" || [SLIDSCA] =="2") && ([SHOW_BADDEB] == "No" || [BADDEB] =="2" ) )
HardCheck("ADDITIONAL PAYMENT UNSPECIFIED: You must select at least one reason for underpayment.");
-
if ( [MOREPAY] =="1" && [EPAYPAT] =="2" && [EPAYCAR] =="2" && [EPAYAID] =="2" && [EPAYPINS] =="2" && [EPAYVA] =="2" && [EPAYCHAM] =="2" &&
[EPAYWORK] =="2" && [EPAYOTH] =="2" ) )
HardCheck("ADDITIONAL PAYMENT UNSPECIFIED: You must select at least one reason for underpayment.");
if ( [MOREPAY] =="1" && [EPAYPAT] =="2" && [EPAYCAR] =="2" && [EPAYAID] =="2" && [EPAYPINS] =="2" && [EPAYVA] =="2" && [EPAYCHAM] =="2" &&
[EPAYWORK] =="2" && [EPAYOTH] =="2" ) )
HardCheck("ADDITIONAL PAYMENT UNSPECIFIED: You must select at least one reason for underpayment.");
if ( [ELIGVET2] =="2" && [EPAYPAT] =="2" && [EPAYCAR] =="2" && [EPAYAID] =="2" && [EPAYPINS] =="2" && [EPAYVA] =="2" && [EPAYCHAM] =="2" &&
[EPAYWORK] =="2" && [EPAYOTH] =="2" ) )
HardCheck("PAYMENT UNSPECIFIED: You must select at least one reason for underpayment.");
IF C5 < C2 then show C6 Adjustments or Discount response options a-h, and C6 Expecting additional payment options i-p. If C5 > C2 then show C6 Payments more than charges. When C2 recorded -5s only, skip PLC1, C6_Additional, ADJEXTRA, and go to LSPCHECK.
C6 - (DATE) should fill based on the following logic:
IF MREVTYPE (A1 of Hospital Medical Event Form) = 1 or 5, fill “ INPATBEG_DAT” (A2a of Hospital Medical Event Form).
IF MREVTYPE (A1 of Hospital Medical Event Form) = 2, 3, or 4, fill “OUTPAT_DATE” (A2c of Hospital Medical Event Form).
(less than/more than) – [If MREVTYPE=2,3, or 4: If C5 < C2 fill: "less than", else if C5 > C2 fill: "more than".
If MREVTYPE=1 or 5: If C5 < C2a fill: "less than", else if C5 > C2a fill: "more than".]
DK/REF – [If MREVTYPE=2,3, or 4 GO TO BOX 3. If MREVTYPE=1 or 5 GO TO FINISH SCREEN.]
DO NOT SHOW Q6_Exceeded if any selection on form UNDERPAYMENT (e.g., any entry of 1 or “YES”)
C6p, should each be set up as a question loop that will require:
A HISTORY BOX to display responses already collected.
A question to appear after each iteration of the question that reads: Any more expected payments? YES=1 NO=2
The “something else” option should be set up so a response can be selected from a list, or entered in as text.
C6p - The EPAYOTOSTXT variable was added to record free-form text for the “Other, Specify” option. Interviewers will be able to record responses in the text box that do not occur in the listed options. DCS instructions onscreen for EPAYOTOSTXT read “EXPECTING ADDITIONAL PAYMENT,” and ““PLEASE SPECIFY OTHER.” EPAYOTOSTXT field is 50 characters.
Other
C6p – Include the following options in listed options for the “Other Specify”;
Auto or Accident Insurance
Indian Health Service
State Public Mental Plan
State/County/Local Program
Other
ALSO ALLOW SYSTEM TO PULL UP NAME OF SOURCE SPECIFIED IN C4h.
2019 UPDATE: Each C6_additional item i-p (EPAYPAT to EPAYOTH) appears on its own screen, along with the entire C6_additional question text. The differences among screens is only the source of additional expected payment being asked about.
2019 UPDATE: IF PLC1 ITEMS DISADJ, MOREPAY, SLIDSCA2, BADDEB2, AND ELIGVET2 ALL = 2, AND C6_ADDITIONAL ITEMS EPAYPAT, EPAYCAR, EPAYAID, EPAYPINS, EPAYVA, EPAYCHAM, EPAYWORK, AND EPAYOTH ALL =2, DISPLAY HARDCHECK: “YOU MUST SELECT AT LEAST ONE REASON PAYMENTS ARE LESS THAN CHARGES. RETURN TO PLC1 ITEMS AND/OR C6_ADDITIONAL ITEMS AND SELECT THE REASON(S).”
2019 UPDATE: IF ADJEXTRA = 2, DISPLAY A HARD CHECK: “IF THE ANSWER IS ‘NO,’ PLEASE GO BACK TO C5 (VERIFY TOTAL PAYMENTS) TO RECONFIRM CHARGES AND PAYMENTS AS NEEDED.”
EDIT SPECS FROM WESTAT
QC6 REASONS FOR PAYMENTS LESS THAN CHARGES Follow Skip Pattern
DATA ITEM |
SPECIFICATIONS |
ACTION, if specification not met |
QC6 a – r Reason for PAYMENTS LESS THAN CHARGES
See QC4-QC6 CONSISTENCY notes
|
If payments are less than charges, there must be a YES (1) answer on lines a – r. |
Blue Sheet, if there is no YES answer, and payments are less than charges. |
The answer must be consistent with the source of payments on QC4. |
Check the answer with the QC4 – QC6 CONSISTENCY reference sheet, or page 5-34 of the spex. |
|
YES (1) or NO (2) must be circled for each choice. Since YES (1) may be answered for more than one choice, only the TRC can answer NO (2). |
Blue Sheet if missing for any choice. Blue Sheet if both YES (1) and NO (2) are circled for a choice. |
|
Blue Sheet if only YES answer is circled, and NO answers are blank, and the payments are less than charges. Let the TRC fill in the NO answers. |
||
If there is a YES answer in PAYMENTS MORE THAN CHARGES section, all choices in the PAYMENTS LESS THAN CHARGES SECTION should be NO (2). |
Blue Sheet if there is a YES answer in both PAYMENTS LESS and PAYMENTS MORE sections. |
|
Circle NO (2) for all answers in the PAYMENTS LESS section, if all answers are blank and there is a YES (1) answer in the PAYMENTS MORE section. |
||
If OTHER is answered, there must be an answer on the SPECIFY line (QC6 line h or line p). Sometimes the answer is written outside the line, as a comment.
Answer on the SPECIFY line (QC6 line h or line p) needs review. |
Check Decision log for all Specify answers. If it is on the Decision log, follow directions given there. If the answer is not there, Yellow Sheet. |
|
Blue Sheet if Specify answer is missing. |
||
If the answer is written outside of the Specify line, and it is on the Decision Log, circle the answer to indicate that it should be Caded. Yellow Sheet if it is not on the Decision Log. |
||
QC6 line h answers should also be reflected in QC4 unless total pay is $0.00. State program paid; State program adj. Exceptions :Hospital w/o or sm ball adj |
Yellow Sheet. |
|
Provider write-off and Small balance write-off are acceptable answers on line h. |
Accept. |
|
Courtesy Discount (line d) may need review. |
If the only payer is an insurance, Yellow Sheet. |
|
If there are three insurance types, managerial review is needed. |
If the sources of payment include three or more insurance types, Yellow Sheet. This may be indicated by the answers to QC4 and QC6 in all books for a patient. |
|
Adjustments are acceptable with no payment from that source in QC4. |
Accept, unless it looks like wrong answer was circled. For example, QC4 says Medicare paid $0.00; QC6 says Medicare adjustment or limit. |
|
Comments may need review. |
Check the Decision Log. Follow instructions. It may be permissible to move the comment to QC6 (line h or p). |
|
If Comments say “in collections” expect that the answer to QC6 will be Expecting Patient Payment or Bad Debt. |
Accept if QC6 is answered “Expecting Payment from Patient” and/or “Bad Debt.” Otherwise, Yellow Sheet. |
|
“In collections” cannot be an answer on the Specify line. If “Expecting Payment from Patient” and/or “Bad Debt” answers are given, cross out “in collections” and change line p to 2 (NO). If these are not answered, Yellow Sheet. |
||
Books should be compared for consistency. |
Review all books for a patient. It is not necessary for books to be identical, but if it looks like the wrong answer was given in a book, Blue Sheet. |
|
There should not be an adjustment in the expecting payments section (line p). |
Blue Sheet if the answer to this question is not a payer source. |
QC6 Reasons for Payments More Than Charges. Follow Skip Pattern
DATA ITEM |
SPECIFICATIONS |
ACTION, if specification not met |
QC6 s – v Reason for PAYMENTS MORE THAN CHARGES
See QC4-QC6 CONSISTENCY notes on page 5- 34.
|
OVERPAYMENTS NEED REVIEW |
Yellow Sheet. |
If payments are more than charges, there must be a YES (1) answer on lines s-v |
Blue Sheet. |
|
More than one YES answer is acceptable. |
Blue Sheet if the NO answers are missing and payment is more than charges. |
|
The answer must be consistent with the source of payments on QC4. |
Check the answer with the QC4 – QC6 CONSISTENCY notes on page 5-34. |
|
YES (1) or NO (2) must be circled for each choice. |
Blue Sheet if missing and payment is less than charge. |
|
Since YES (1) may be answered for more than one choice, only the TRC can answer NO (2). |
Blue Sheet if only YES answer is circled, and the NO answers are blank, if payments are more than charges. Let the TRC fill in the NO answers. |
|
If there is a YES answer in PAYMENTS LESS THAN CHARGES section, all choices in the PAYMENTS MORE THAN CHARGES SECTION should be NO (2).
Review the payments and charges. Are payments less or more than charges? |
Blue Sheet if there is a YES answer in both PAYMENTS LESS and PAYMENTS MORE sections. |
|
If Payments are Less than Charges, and answers in the PAYMENTS MORE section are all blank, and there is a YES (1) answer in the PAYMENTS LESS section,. Circle NO (2) for all answers in the PAYMENTS MORE section. |
||
If OTHER is answered, there must be an answer on the SPECIFY line (QC6 line v). Sometimes the answer is written outside the line, as a comment.
Answer on the SPECIFY line (QC6 line v) needs review. |
Check Decision log for all Specify answers. If it is on the Decision log, follow directions given there. If the answer is not there, Yellow Sheet. |
|
Blue Sheet if Specify answer is missing. |
||
If the answer is written outside of the Specify line, circle the answer if it is on the Decision Log. Yellow Sheet if it is not on the Decision Log. |
||
If there are three insurance types, review is needed. |
If the sources of payment include three or more insurance types, Yellow Sheet. This may be indicated by the answers to QC4 and QC6 in all books, looked at together. |
|
OTHER/SPECIFY answers in QC6 line v should be reflected in an OTHER/SPECIFY answer in QC4 State program paid; State program adj |
Yellow Sheet.
|
QC4 AND QC6 CONSISTENCY NOTES
Compare QC4 and QC6
PAYER IN QC4 |
ANSWER TO QC6 |
Medicare |
Accept any of these alone: Medicare Adjustment, Contractual Arrangement, Expecting Payment from any source, Charity, or Bad Debt. Accept Medicare Adjustment plus any of the following: Medicaid Adjustment, Contractual Arrangement, Courtesy Discount, Expecting Payment from any source, Charity or Bad Debt. If Insurance Write-Off is answered, Yellow Sheet. If the only answer is an adjustment or limit or arrangement other than Medicare, look for an indication* that this other source is involved. If no indication, Blue Sheet. |
Medicaid |
Accept any of these alone: Medicaid Adjustment; Expecting Payment from any source, Charity, or Bad Debt. Accept Medicaid Adjustment plus any of the following: Medicare Adjustment, Contractual Arrangement, Courtesy Discount, Expecting Payment from any source, Charity or Bad Debt. If Insurance Write-Off is answered, Yellow Sheet. If the only answer is any adjustment or limit or arrangement other than Medicaid, look for an indication* that the other source is involved. If no indication, Blue Sheet. |
Private Insurance |
Accept any of these alone: Contractual Arrangement; Expecting Payment from any source, Charity, or Bad Debt. Accept Contractual Arrangement plus any of the following: Medicare Adjustment, Medicaid Adjustment, insurance w/o, Courtesy Discount, Expecting from any source, Charity or Bad Debt. If only answer is any adjustment or limit other than Private Insurance, look for indication* that the other source is involved. If no indication, Blue Sheet. |
TRICARE, Champus, ChampVA |
Accept anything that is acceptable for Private Insurance, and/or accept Eligible Veteran or OTHER/SPECIFY: Tricare Adjustment or Champus Adjustment. May be the primary insurance or secondary to other kinds of insurance. |
VA or Indian Health |
Usually says “ELIGIBLE VETERAN” or OTHER/SPECIFY: “ELIGIBLE…” There may be no payment or payment by any source. If there is a payment by another source, QC6 may refer to that source, either alone or in addition to Eligible Veteran (or Other/Specify “Eligible…” answer. If Insurance Write-Off is answered, Yellow Sheet. Accept Courtesy Discount, Charity and Bad Debt in addition to “Eligible…” or other insurance adjustment. |
Workers’ Comp
|
Should say “Workers’ Comp Adjustment.” If missing, Blue Sheet. Accept Courtesy Discount, Charity and Bad Debt in addition to Workers’ Comp Adjustment. If Insurance Write-Off is answered, Yellow Sheet. Expect that no other insurance will be involved. If Workers’ Comp is given with any other insurance, Yellow Sheet. |
Look for INDICATIONS OF ADDITIONAL SOURCES OF PAYMENT in:
QC4 (payers) in other books
Comments
Expecting Payment section
 DECISION
LOG FOR QC6
DECISION
LOG FOR QC6
PROGRAMMER NOTES: Include all “Problems” in a drop down menu at the other specify entry and program the required “decision” behind the scenes. May require implementing instructional boxes for the DCS/abstractor. For example, if the DCS selects “insurance was never billed” an instruction box should pop up asking the DCS to probe to include type of insurance if know, such as MEDICARE NEVER BILLED
Problem |
Decision / Categorization |
Payment Less than Charges |
If instructions say to add
an answer to line h or line p, change the YES/NO answer to 1 and
cross out the answer 2. |
Underpayment exists in Q(C4) by a State (or Federal, or County, or City) Plan ---- Plan may be Fund, Program, Grant ------ type of plan may be given ------- REMOVE Name of State if it is present |
Code in 'OTHER' as (name of source given in Q(C4h)). |
Examples: |
|
Nevada State Disability |
State Disability. |
State Breast Cancer Program |
State Breast Cancer Program. |
Maryland Indigent Program |
State Indigent Program. |
Federal Grant |
Federal Grant. |
Cook County Indigent Fund |
County Indigent Fund. |
State Program |
State Program. |
Zero total payment in Q(C4) but comment about a State (or Federal, or County, or City) Plan ---- Plan may be Fund, Program, Grant ------ type of plan may be given ------- REMOVE Name of State if it is present |
If TRC says Charity care,
accept as is. |
Comment says that insurance was never billed |
Code in 'Other' (line h) as
NEVER BILLED. |
Comment says Insurance denied payment. |
Code in 'Other' (line h) as
INSURANCE DENIED. |
Comment mentions billing error. |
Code in 'Other' (line h) as
Billing Error. |
Comment mentions untimely filing, billed late. |
Code in 'Other' (line h) as
Billed Late. |
Comment mentions Insurance denied, with an amount, such as Private Insurance denied $52.50. |
Code in 'Other' (line h) as
INSURANCE DENIED. |
Comment mentions that the insurance doesn't cover a procedure. |
Code in 'Other' (line h) as
INSURANCE DENIED: PROCEDURE NOT COVERED. |
Comment mentions that insurance doesn't cover if no pre-authorization |
Code in 'Other' (line h) as
INSURANCE DENIED: NO PRE-AUTHORIZATION. |
Comment mentions nurse visit not covered |
Code in 'Other' (line h) as
INSURANCE DENIED: NURSE VISIT. |
Comment says patient paid the deductible. |
Do not code in 'Other'
(line h). |
Comment says insurance made an adjustment. |
Do not code in 'Other'
(line h). |
Comment mentions Collection Agency or " in Collections" |
Do not code in 'Other' line
h or line p. |
Collection Agency or "in collections" is Other/Specify answer (line h or line p) |
Cross out "in
collections," etc. as the 'Specify' answer (line h or line
p). |
Small balance w/o (Small balance write off) |
Code in Other as Small Balance W/O |
Small balance Adj (Small balance adjustment) |
Code in Other as Small balance Adj |
Military |
Blue Sheet for more specific information |
Dependent of active duty military / Active duty military dependent |
Code in 'other' as Eligible Active Duty Fam Mem |
Active duty armed forces member / Active duty military |
Code in 'Other' as Eligible Active Duty |
Active duty family member |
Code in 'Other' as Eligible Act Duty Fam Mem |
Retired veteran / Retired military |
Code in 'Other' as Eligible Retiree |
Retired veteran's family member |
Code in 'Other' as Eligible Retiree Fam Mem |
Retired Military Dependent |
Code in 'Other' as Eligible Retiree Fam Mem |
Veteran's family member |
Code in 'Other' as Eligible Veteran Fam Mem |
Indian Health |
Code in 'Other' as Eligible Native American |
Clerical fee; administrative fee |
YELLOW SHEET |
Grant - DK who is funding it |
Code in 'Other' as Grant - DK who is funding it. |
HMO |
Blue Sheet for type of insurance: Medicare, Medicaid, or Private, other |
Comment says No payments due to Federal Vaccines given |
Code in 'Other' (line h) as Federal Vaccine Program. |
Payment More than Charges |
Yellow Sheet ALL OVERPAYMENTS |
Tricare (or Champus) payment exceeds charges |
Accept Private Insurance adjustment or, in 'OTHER', as Tricare (or Champus) Adjustment |
Overpayment exists in Q(C4) by a State (or Federal, or County, or City) Plan ---- Plan may be Fund, Program, Grant ------ type of plan may be given ------- REMOVE Name of State if it is present |
Code in 'OTHER' as (name of source given in Q(C4h)). |
Examples: |
|
Nevada State Disability |
Code in 'Other' (line v) as State Disability. |
State Breast Cancer Program |
Code in 'Other' as State Breast Cancer Program. |
Maryland State Indigent Program |
Code in 'Other' as State Indigent Program. |
Federal Grant |
Code in 'Other' as Federal Grant. |
Cook County Indigent Fund |
Code in 'Other' as County Indigent Fund. |
State Program |
Code in 'Other' as State Program. |
Comment mentions Patient Credit, Patient Overpayment; Patient has a balance |
Yellow Sheet. |
SECTION 17 – LUMP SUM PAYMENTS
[Page 26 – lump sum payments (1 of 4)]
LSPCHECK WAS THIS EVENT COVERED BY A LUMP SUM?
YES
NO
PROGRAMMING NOTE:
DK/REF: GO TO FINISH
IF (all source of payment fields PATPAYM to WORKPAYM and OTHRPAYM have entries of 0.00) or (TOTLPAYM is 0.00 or missing)
AND a-e = NO ( DISADJ, MOREPAY, SLIDSCA2, BADDEB2, ELIGVET2) AND i-p = NO (EPAYPAT, EPAYCAR, EPAYIAD, EPAYPINS, EPAYVA, EPAYCHAM, EPAYWORK, EPAYOTH ) AND (LSPCHECK=”No”) display a hard error at LSPCHECK, “PAYMENT VALIDATION FAILED: No payment source or reason(s) identified. Return to Sources of Payment or Payments NE Charges, or record Lump Sum Payment here.” This hard error will require user to correct one of those conditions or break off the event form
SECTION 18 – PATIENT ACCOUNTS – CAPITATED BASIS
NOTE: See end of section for edit specs from Westat for questions C7a, C7b, C7c, C7d, C7e, and C7f.
[Page 30– PATIENT ACCOUNTS - CAPITATED BASIS (1 of 4)]
SCREEN LAYOUT
PROGRAMMER NOTES
C7a – (this visit/these visits/this stay) – [If MREVTYPE = 2, 3, or 4 and GLOFEE (A5a) = YES fill: "these visits". If MREVTYPE = 2, 3, or 4 and GLOFEE (A5a) = NO fill: "this visit". If MREVTYPE = 1 or 5 fill: “this stay”.]
C7a(g) - The COVOTOSTXT variable was added to record free-form text for the “Other, Specify” option. Interviewers will be able to record responses in the text box that do not occur in the listed options. COVOTOSTXT field allows up to 50 characters. Screen reads: “OTHER INSURANCE PLAN…” “PLEASE SPECIFY OTHER”.
C7a(g) is a question loop that will require:
(1) A HISTORY BOX to display responses already collected.
(2) A question to appear after each iteration of the question that reads: Any more plans? YES=1 NO=2
(3) The “something else” option should be set up so a response can be selected from listed options, or entered in as text.
C7a(g) – Include the following options for the “Other Specify”;
Auto or Accident Insurance
Indian Health Service
State Public Mental Plan
State/County/Local Program
Other
C7b – (this visit/these visits/ any part of this stay) – [If MREVTYPE = 2, 3, or 4 and GLOFEE (A5a) = YES fill: "these visits". If MREVTYPE = 2, 3, or 4 and GLOFEE (A5a) = NO fill: "this visit". If MREVTYPE = 1 or 5 fill: “any part of this stay”.]
C7b - [IF ANYCOPAY=2 GO TO C7e]
C7a - DK/REF – CONTINUE TO C7b
C7b - DK/REF – GO TO C7e
2021 UPDATE: IF C7a a-g (COVCARE, COVAID, COVPINS, COVVA, COVCHAM, COVWORK, COVOTHR) all equal 2 (NO), display soft check:
YOU HAVE INDICATED CAPITATED PAYMENT, BUT ENTERED ‘NO’ FOR ALL INSURANCE TYPES. PLEASE CHECK THE RECORDS AGAIN AND/OR PROBE WITH THE POC TO DETERMINE THE INSURANCE PLAN(S) TYPE THAT COVERED THIS EVENT, AND CHANGE THE ANSWER FOR THAT ITEM. OR CLICK ‘SUPPRESS’ TO CONTINUE.
2019 UPDATE: Each C7a item a-g (COVCARE to COVOTHR) appears on its own screen, along with the entire C7a question text. The differences among screens is only the payer type (Medicare, Medicaid, etc.).
[Page 31– PATIENT ACCOUNTS - CAPITATED BASIS (2 of 4)]
SCREEN LAYOUT
[Page 32– PATIENT ACCOUNTS - CAPITATED BASIS (3 of 4)]
SCREEN LAYOUT C7e. Do your records show any other payments for (this visit/these visits/this stay)? |
YES=1, NO=2 OTHPAY |
PROGRAMMER NOTES
(this visit/these visits/this stay) – I[f MREVTYPE = 2, 3, or 4 and GLOFEE (A5a) = YES fill: "these visits". If MREVTYPE = 2, 3, or 4 and GLOFEE (A5a) = NO fill: "this visit". If MREVTYPE = 1 or 5 fill: “this stay”.]
DK/REF – [If MREVTYPE = 2, 3, or 4 GO TO BOX 3. If MREVTYPE = 1 or 5 GO TO FINISH SCREEN.]
IF OTHPAY=2: [If MREVTYPE = 2, 3, or 4 GO TO BOX 3. If MREVTYPE = 1 or 5 GO TO FINISH SCREEN.] |
|
[Page 33– PATIENT ACCOUNTS - CAPITATED BASIS (4 of 4)]
SCREEN LAYOUT
C7f. From which of the following other sources has the facility received payment for (this visit/these visits/this stay) and how much was paid by each source? Please include all payments that have taken place between (DATE) and now for this visit.
RECORD PAYMENTS FROM APPLICABLE PAYERS
[DCS ONLY] IF NAME OF INSURER, PUBLIC, OR HMO, PROBE: And is that Medicare, Medicaid, or private insurance?
|
SOURCE a. Patient or Patient’s Family; b. Medicare; c. Medicaid; d. Private Insurance; e. VA/ChampVA; f. Tricare; g. Worker’s Comp; or h. Any more sources? (IF SOMETHING ELSE: What was that?) OTHOTOS OTHOTOSTXT |
PAYMENT AMOUNT $OTHPAT $OTHCARE $OTHAID $OTHPINS $OTHVA $OTHCHAM $OTHWORK
$OTHOTHR
|
PROGRAMMER NOTES
C7f: Each of the fields requires a non-blank entry, as was done for C4 sources of payment. Entries of 0, DK, RF are allowed here.
C7f - (DATE) should fill based on the following logic:
IF MREVTYPE (A1 of Hospital Medical Event Form) = 1 or 5, fill “INPATBEG_DAT” (A2a of Hospital Medical Event Form).
IF MREVTYPE (A1 of Hospital Medical Event Form) = 2, 3, or 4, fill “OUTPAT_DATE” (A2c of Hospital Medical Event Form).
(this visit/these visits/this stay) – I[f MREVTYPE = 2, 3, or 4 and GLOFEE (A5a) = YES fill: "these visits". If MREVTYPE = 2, 3, or 4 and GLOFEE (A5a) = NO fill: "this visit". If MREVTYPE = 1 or 5 fill: “this stay”.]
C7f(h) - The OTHOTOSTXT variable was added to record free-form text for the “Other, Specify” option. Interviewers will be able to record responses in the text box that do not occur in the listed options. Field allows up to 50 characters.
C7f(h) OTHOTOSTXT screen text: “OTHER PAYMENT SOURCE…” “PLEASE SPECIFY OTHER”.
(h) is a question loop that will require:
A HISTORY BOX to display responses already collected.
A question to appear after each iteration of the question that reads: Any more sources? YES=1 NO=2
The “something else” option should be set up so a response can be selected from listed options, or entered in as
text.
(h) – Include the following options in listed options for the “Other Specify”;
Auto or Accident Insurance
Indian Health Service
State Public Mental Plan
State/County/Local Program
Other
DK/REF – [If MREVTYPE = 2, 3, or 4 GO TO BOX 3. If MREVTYPE = 1 or 5 GO TO FINISH SCREEN.]
After C7f: [If MREVTYPE = 2, 3, or 4 GO TO BOX 3. If MREVTYPE = 1 or 5 GO TO FINISH SCREEN.]
2019 UPDATE: Each C7f item a-g (OTHPAT to OTHWORK) appears on its own screen, along with the entire C7f question text. The differences among screens is only the payer type (Patient or Patient’s Family, Medicare, etc.).
EDIT SPECS FROM WESTAT
QC7 CAPITATED BASIS. Follow Skip Pattern
DATA ITEM |
SPECIFICATIONS |
ACTION, if specification not met |
|
||
|
Capitated Section
Completed if QC3 is Capitated (2).
|
Entire Capitated Section cannot be DK or RF. |
Blue Sheet, to verify that Reimbursement type is Capitated. |
||
|
DK or RF is acceptable for individual answers in the Capitated Section, as long as entire section is not DK or RF. |
Accept DK or RF. Change to -7 or -8. Yellow Sheet, if questionable. |
|||
|
QC7a – Capitated – what kind of insurance |
Must be completed if Reimbursement Type in QC3 = Capitated Basis |
Blue Sheet, if no answers are YES (1). |
||
|
More than one answer of YES is acceptable. |
Blue Sheet, if the NO (2) answers are not circled, and there is a YES (1) answer. |
|||
|
Answers should agree in all books for a pair. |
Yellow Sheet, if answers differ in books for a pair. |
|||
|
If SOMETHING ELSE is answered, there must be an answer on the SPECIFY line. |
Blue Sheet if missing. |
|||
|
Answer on the SPECIFY line needs review. |
Check Decision log. If it is on the Decision log, follow directions given there. If the answer is not there, Yellow Sheet. |
|||
|
“HMO,” “Public,” or the name of an insurance company is not acceptable as a SPECIFY answer. |
Blue sheet, asking which type of insurance. Note: the same insurance company can provide private insurance and also administer Medicare and/or Medicaid payments. |
|||
|
If “HMO, DK type” Yellow Sheet. |
||||
|
QC7b – Any Co-pay |
1 or 2 circled must be circled. |
If blank and there is no indication of a co-payment, circle NO (2). |
||
|
QC7c - Co-payment amount |
If QC7b is YES, there must be an amount. |
Blue Sheet. |
||
|
Co-pay range is typically > 0 and <=$50. |
Yellow Sheet. |
|||
|
Co-pay amount is typically a whole dollar number. |
Yellow Sheet. |
|||
|
DK or RF is acceptable. |
Change DK to – 8. Change RF to – 7. |
|||
|
If payment by patient is $1.00 or less, expect that the insurance type will be a public type – Medicare, Medicaid, state program, etc. |
Yellow Sheet if there is another insurance type indicated. |
|||
|
QC7d - Co-payment payer |
If QC7b is YES, there must be a co-payer source. |
Blue Sheet. |
||
|
Sources other than patient or patient’s family need review. |
Yellow Sheet if source of co-pay is not patient or patient’s family. |
|||
|
Answers of more than one source need review. |
Yellow sheet. |
|||
|
Answer on the SPECIFY line needs review. |
Check Decision log. If it is on the Decision log, follow directions given there. If the answer is not there, Yellow Sheet. |
|||
|
“HMO,” “Public,” or the name of an insurance company is not acceptable as a SPECIFY answer. |
Blue sheet, asking which type of insurance. Note: the same insurance company can provide private insurance and also administer Medicare and/or Medicaid payments. |
|||
|
QC7e Capitated Secondary Payment? |
Must be answered 1 (YES) or 2 (NO). |
If blank and nothing indicates that there is a Capitated Secondary payment, Circle 2 (NO). |
||
|
Capitated Secondary Payments need review. |
Yellow Sheet if YES. |
|||
|
QC7f – Source(s) and amount of payment for CAPITATED SECONDARY PAYMENT |
If QC7e is YES (1), a payment amount must be filled in for at least one source. |
Blue Sheet, if there is no amount given. |
||
|
If there is an amount, the Capitated Secondary Payment needs special review. |
Yellow Sheet all Capitated Secondary Payments. |
|||
|
DK or RF is acceptable. |
Change DK to –8 and RF to –7; Yellow Sheet as a Capitated Secondary Payment. |
|||
|
If question is not skipped (QC7e is YES), all sources of payment must have a dollar value. |
If there is a dollar amount for one source, fill in $0.00 for all the other sources. Do not leave any lines blank, unless the question is skipped (when QC7e is NO). |
|||
|
Answer on the SPECIFY line (h) needs review. |
Check Decision log. If it is on the Decision log, follow directions given there. If the answer is not there, Yellow Sheet. |
|||
|
“HMO,” “Public,” or the name of an insurance company is not acceptable as a SPECIFY answer. |
Blue sheet, asking which type of insurance. Note: the same insurance company can provide private insurance and also administer Medicare and/or Medicaid payments. |
|||
|
Note: There is no Total Payments field for this question. |
If the TRC has written the Total Secondary Capitated Payment on the last line (for Other/Specify payment), cross it out. |
|||
Decision Log for C7a C7d, and C7f (same as Decision Log for QC4)
PROGRAMMER NOTES: Include all “Problems” in a drop down menu at the other specify entry and program the required “decision” behind the scenes. May require implementing instructional boxes for the DCS/abstractor. For example, if the DCS selects “vocational rehabilitation” an instruction box should pop up asking the DCS to probe for source of funding: federal, state, county, other gov’t, private, etc.]
Problem |
Decision / Categorization |
Source of Payments |
|
State (or Federal, or County, or City) Plan ---- Plan may be Fund, Program, Grant ------ type of plan may be given ------- REMOVE Name of State if it is present |
Code by indicating source
of funds, then type of plan if given |
Examples: |
|
Nevada State Disability (SRS) |
Code in 'Other' as State Disability |
State Breast Cancer Program |
Code in 'Other' as State Breast Cancer Program |
Maryland Indigent Program |
Code in 'Other' as State Indigent Program |
Federal Grant |
Code in 'Other' as Federal Grant |
Cook County Indigent Fund |
Code in 'Other' as County Indigent Fund |
State Program |
Code in 'Other' as State Program |
Comment indicates one of the above, but it is not indicated in QC4 (line h) |
Yellow Sheet |
Comment indicates the name of an insurance company for QC4. |
Ignore the name of an insurance company if we have the type of insurance payer. |
QC4 (line h) 'Specify' answer is name of an insurance company |
Blue Sheet to determine source of funding: Federal, State, County, Other gov't, Private etc |
Children's Special Services |
Blue Sheet to determine source of funding: Federal, State, County, Other gov't, Private etc |
Vocational Rehabilitation |
Blue Sheet to determine source of funding: Federal, State, County, Other gov't, Private etc |
Welfare |
Blue Sheet to determine source of funding: Federal, State, County, Other gov't, Private etc |
Hospital Fund |
Blue Sheet to determine source of funding: Federal, State, County, Other gov't, Private etc |
Grant |
Blue Sheet to determine source of funding: Federal, State, County, Other gov't, Private etc |
Grant - DK who is funding it |
Code in 'Other' as GRANT - DK FUNDING |
Breast Cancer Program |
Blue Sheet to determine source of funding: Federal, State, County, Other gov't, Private etc |
Indigent Program or Fund for Indigents |
Blue Sheet to determine source of funding: Federal, State, County, Other gov't, Private etc |
Local |
Blue Sheet to determine who is funding it , I.e. State, County, City, Other gov't, etc |
MediCal (in California) |
Code as Medicaid (C4c) |
Employer |
Yellow Sheet |
Verbiage about car/auto accident paid or auto/car insurance paid |
Code in Other as Auto Insurance |
Military |
Blue Sheet for more specific information |
Indian Health |
Code in Other as Indian Health Service |
CHDP; CHIP |
Accept, but cross out any state or county name |
WIC |
Accept, but cross out any state or county name |
AARP (American Association of Retired Persons) |
Code as Private Insurance (QC4d) |
Prepaid Mental Health Plan - State Plan |
Code In Other as State Public Mental |
HMO |
Blue Sheet to find out Insurance Type: Medicare, Medicaid, Priv Ins., Other; Ask for source of payment. |
[Page 34– BILLING RECORDS – BRF SUMMARY]
SCREEN LAYOUT
1. What is the name of the PA form received from the provider?
Form Name
ID
2. Rate the quality and completeness of the following billing information provided with this form:
Global Fee
CPT4/Services and Charges
Reimbursement Type
Source of Payment by Reimbursement Type
Total Payment by Reimbursement Type
Adjustments by Reimbursement Type
Expecting Additional Payment by Payment Source (including copayment or additional payment information)
Lump Sum Payment
|
BRF_Name
BRF_ID
COMPLETE=1, PARTIAL=2, MISSING = 3, N/A = 4 BRF_GlobalFee COMPLETE=1, PARTIAL=2, MISSING = 3, N/A = 4 BRF_ServiceChgs COMPLETE=1, PARTIAL=2, MISSING = 3, N/A = 4 BRF_Reimbursement COMPLETE=1, PARTIAL=2, MISSING = 3, N/A = 4 BRF_SourceOfPmt
COMPLETE=1, PARTIAL=2, MISSING = 3, N/A = 4 BRF_TotalPmt COMPLETE=1, PARTIAL=2, MISSING = 3, N/A = 4 BRF_Adjustments COMPLETE=1, PARTIAL=2, MISSING = 3, N/A = 4 BRF_Additional
COMPLETE=1, PARTIAL=2, MISSING = 3, N/A = 4 BRF_LumpSum
|
|
BOX 3 [PROGRAM BEHIND THE SCENES – SHOULD NOT APPEAR ON SCREEN. VARIABLE NAME=GOTORVIS] GLOBAL FEE SITUATION (A5a=YES) 1 (GO TO FINISH SCREEN.) RECORDED 5 OR FEWER EVENTS 2 (GO TO FINISH SCREEN.) RECORDED 6 OR MORE EVENTS 3 (GO TO FINISH SCREEN)
|
PROGRAMMER NOTES
DK/REF – Not Applicable here
First screen of this section, Screen BRF_SOURCE, asks DCS to “SELECT BRF SOURCE.” OPTIONS ARE: 1. “ENTER NEW BRF INFO,” 2. “SELECT EXISTING BRF,” AND 3. “BYPASS BILLING FORM.”
On BRF_SOURCE screen, do not display option 2 (SELECT EXISTING BRF) if no BRF information has been entered for any event in the contact group.
If no BRF info has been entered for any event in the contact group display this note on BRF_SOURCE: Note: There are no BRFs currently associated with this Event, please Enter New or Bypass.
If one or more completed events in the contact group have had BRF questions answered, display option 2 on BRF_SOURCE.
Selecting option 2 allows user to select from a menu of BRFs previously entered for other events within the same contact group. The selected form will fill in PAFORM, and all answers associated with that form will fill answers in the BRF section.
Option 3 on BRF_SOURCE GO TO review (RIV1 screen).
EDIT SPECS FROM WESTAT
BOX 3 Follow Skip Pattern
DATA ITEM |
SPECIFICATIONS |
ACTION, if specification not met |
|
BOX 3 Is event a Global fee? Or is the event one that may have a repeat visit?
|
1, 2, or 3 must be circled. |
If blank, answer as below. |
|
If 1=GLOBAL FEE SITUATION is circled, there must be a Global Fee. This answer will appear whenever there is a Global Fee, regardless of the book number. |
Check QA5a. Correct the answer, if wrong. If “1,” there cannot be a repeat visit with a global fee. Skip to QA11. |
||
If 2=RECORDED 5 OR FEWER EVENTS is circled, there cannot be a Global Fee. This answer will appear in book numbers 1-5, in every book without a Global Fee. |
Correct the answer, if wrong. If “2,” there cannot be a repeat visit in books 1 - 5. Skip to QA11. |
||
If 3=RECORDED 6 OR MORE EVENTS is circled, there cannot be a Global Fee. This answer will appear in book number 6 or higher, in every book without a Global Fee. |
Correct the answer, if wrong. If “3,” QA7a must be answered. |
||
RIV1
IS THIS EVENT A REPEATED IDENTICAL VISIT (RIV) EVENT? THAT IS, ARE THERE 10 OR MORE ADDITIONAL EVENTS IDENTICAL TO THIS EVENT, EXCEPT FOR THE DATE OF SERVICE?
IF IN DOUBT, ANSWER NO.
1=YES – THIS EVENT HAS AT LEAST 10 REPEATED IDENTICAL VISITS ASSOCIATED WITH IT.
2=NO
RIV2
RECORD THE DATES OF SERVICE FOR WHICH ALL DATA ARE IDENTICAL TO THIS (FILL DATE OF CURRENT EVENT) EVENT, EXCEPT FOR THE DATE OF SERVICE.
PROGRAMMER NOTES
If RIV1 = NO, go to FINISH SCREEN.
For HOSP, If ANYSBDS = 1, skip RIV1 and RIV2.
RIV2: Require minimum of 10 dates, maximum of 200. After 10 dates, a blank followed by an Enter goes to FINISH SCREEN.
RIV1 – DK/REF not allowed for RIV1, but are allowed for RIV2.
2022 UPDATE: Add soft check when YES is selected for RIV1. Soft check reads:
MARK THIS ITEM AS YES ONLY IF ABSTRACTING AND THE EVENT IS AN RIV. IF COMPLETING BY PHONE, OR IF THE EVENT IS NOT AN RIV, CLOSE THIS MESSAGE AND CHANGE ANSWER TO NO. OTHERWISE, SUPPRESS AND CONTINUE.
SECTION 19 – FINISH SCREEN
ENTER 1 TO FINALIZE THIS CASE.
PROGRAMMER NOTES
At this screen, users will enter 1 and Enter to finalize the event form.
OP2-11_HO_EF_v1.0 Page
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| File Title | MEDICAL EXPENDITURE PANEL SURVEY |
| Author | Diana Greene |
| File Modified | 0000-00-00 |
| File Created | 2024-09-24 |
© 2025 OMB.report | Privacy Policy