Att C Disccussion Guide
06_Attachment C_Discussion Guide_Maximizing HIT through Interoperability in VBP.docx
ASPE Generic Clearance for the Collection of Qualitative Research and Assessment
Att C Disccussion Guide
OMB: 0990-0421
THE
URBAN INSTITUTE
CORE
DISCUSSION
GUIDE

OMB #0990-0421
Expires: 10/31/2020
Attachment C. Discussion Guide: MAXIMIZING THE PROMISE OF HEALTH INFORMATION TECHNOLOGY THROUGH THE PROMOTION OF INTEROPERABILITY: VALUE-BASED CARE
Discussion Guide
[To be customized based on stakeholder type being interviewed, including health IT staff, administrators, and clinicians from health care organizations that share patients, organizations that facilitate health information exchange, and other relevant stakeholders]
Instructions for interviewer
The following semi-structured discussion guide is designed to be tailored as appropriate to the professional perspective and knowledge of respondents. Each of the bolded discussion questions will be asked of the respondents, and possible probes for each will be used as needed to obtain additional information or clarification. Due to time constraints, researchers may prioritize and skip some questions.
In a few sites, where there are several stakeholders whom we would like to include in our study, we may conduct small group interviews instead of individual interviews. In those cases, we will use this discussion guide for the small group interviews but will prioritize the most relevant questions for discussion.
Before beginning, interviewers will read the verbal consent script (see Attachment D) to provide information about the study and to ask consent questions for participation in the study and for audio-recording.
Work History/Experience
Can you please tell us about your position and role or responsibility with [employer name]?
Possible probes:
How long have you worked in this position?
What is your role in the organization?
What experience do you have working with integrating data from outside sources to support the delivery of value-based care?
The Current State of Data Integration
To provide us with some context, our first questions are about how your organization integrates and uses data from outside sources.
How long has your organization been working to integrate data from outside sources and what prompted you to start doing this?
What are your organization’s goals for the data you are working to integrate?
Possible probes:
Is the aim to make the data accessible to providers at the point of care to inform treatment decisions or facilitate care coordination?
Or to use for payment or other operational purposes?
For quality improvement/reporting or population health management?
How advanced would you say your organization is in terms of your data integration efforts, and why would you describe it that way?
Possible probes:
When you think of advanced data integration (perhaps what you are working towards), do you first think of how the data is exchanged and stored?
Do you consider it usefulness and accessibility to the end user?
Is there something else you think of?
As part of this project, we’ve developed an initial diagram to display different levels of data integration that we sent to you ahead of time and is labeled “Figure 1. Levels of Data Integration.” Based on your experience, does this make sense to you in terms of what lower and higher levels of data integration might look like? What would you add or change?
F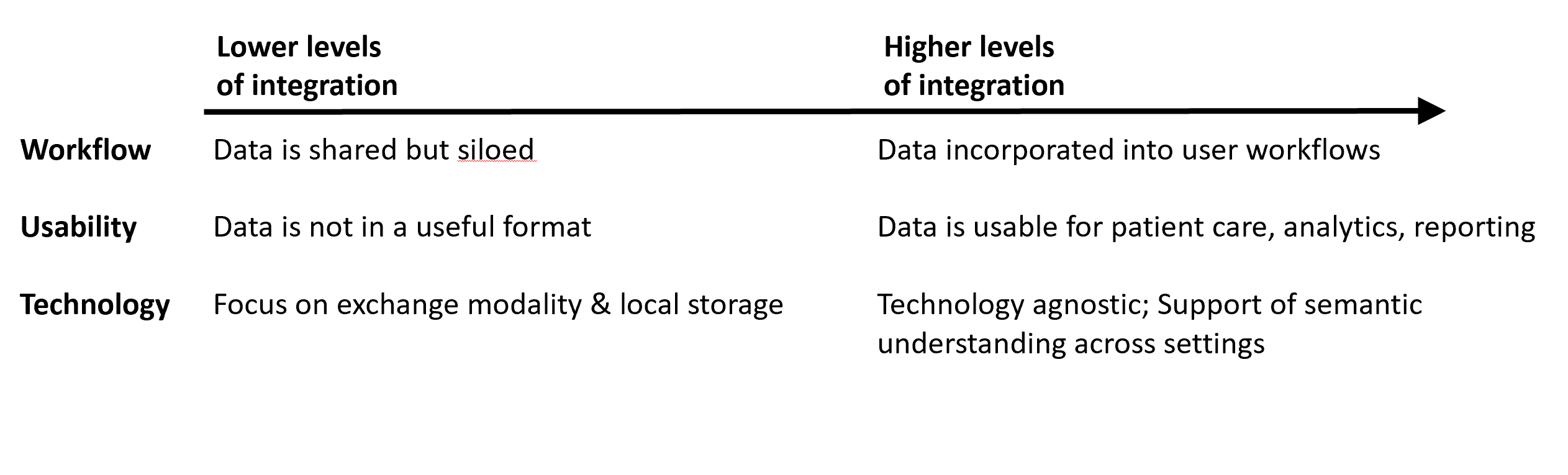 igure
1. Levels of Data Integration
igure
1. Levels of Data Integration
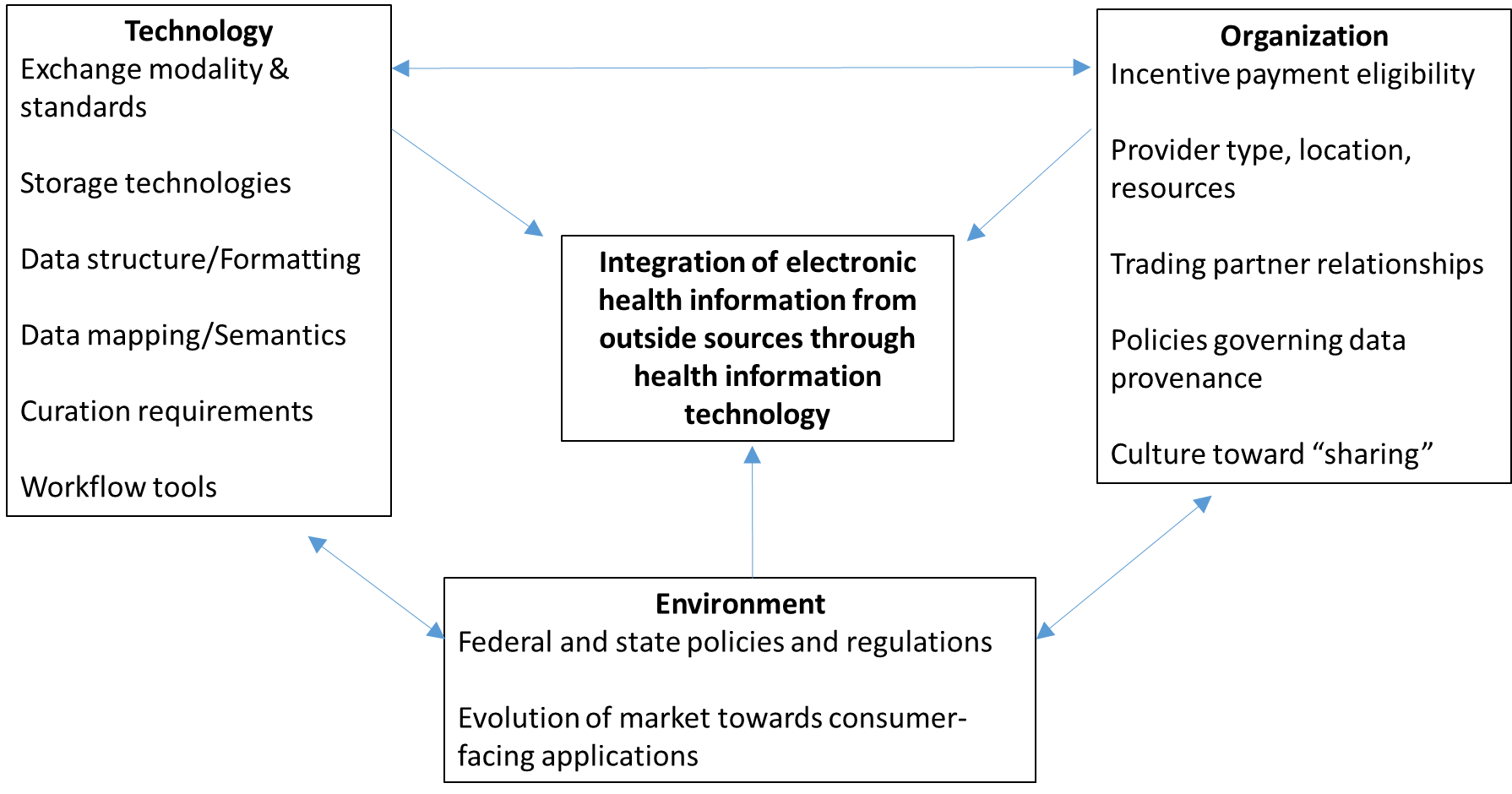
In addition, we’ve been using a technical-organizational-environmental framework to think about the different factors that may be affecting data integration, which are displayed in Figure 2 that we sent to you ahead of time. We will talk through each of these categories individually, but wanted to see at a high level whether you think this captures key factors?
Possible Probes:
Which factors do you see as most important?
Is anything missing that you would add?
Figure 2. Technical, Organizational and Environmental Factors Affecting Data Integration
Technical factors
We will be asking you about technical, organizational, and environmental factors that may be affecting your work to integrate data, starting with technical factors.
What types of data from outside sources are you focused on integrating?
Possible probes:
Are you integrating data from Admit, Discharge, Transfer (ADT) alerts? Summary of care documents? Laboratory results and imaging? Problem List diagnoses, Allergies, Medications and Immunizations (PAMI information)?
How do you obtain the data you integrate into your system?
Possible probes:
a. What are the primary modes of exchange your organization uses? (Direct Secure Messaging, HIOs, vendor networks, eHealth Exchange, or multi-EHR Vendor networks)?
How do you integrate outside data into your system?
Possible probes:
a. How do you parse and map the data?
b. Do you have a process for assuring data quality?
c. How do you store the data?
d. How do you deal with different data structures and formats?
How do end users access the outside data?
Possible probes:
a. Is it integrated into their workflow, or do they have to go to a separate section of the EHR?
b. What format do they see the data in – is it searchable, or an attachment?
c. Can they tell where what was the original source of the data? If yes, how?
How did you incorporate the integrated data into clinical workflows?
Possible probes:
How do you help end users access the right data at the right time and minimize their effort needed to do so?
What have you done to make the data usable to end users? How well has this worked?
What have been the biggest technical challenges with integrating data from outside sources?
Possible Probes:
a. Have HL7 Interface costs been a challenge?
b. How about variation in the use of standards and trading partner capabilities?
c. Have you had challenges with data segmentation requirements to address 42 CFR Part 2?
Organizational factors
The next questions are related to organizational factors affecting data integration.
Are there characteristics of your organization that have facilitated or impeded data integration?
Possible probes:
a. Is your organization type, specialty, location, or level of resources a factor?
Is your organization part of value-based payment arrangements that have incentivized integrating data from outside sources? If yes, how so?
Possible probes:
Are you a part of an ACO?
Do you have alternative payment model contracts that incentive quality, efficiency and/or population health management?
What aspects of these reimbursement models have most incentivized investing in data integration? (Focus in reducing readmissions? Reducing costs? Certain quality measures?)
Are there certain types of referral partners that your organization has focused on integrating data from? If yes, which ones and why?
Possible probes:
How did you identify which partners to prioritize – was it an analytic process such as looking at referral patterns?
Do you focus on other organizations with whom you share accountability for a set of patients?
Do you focus on data from certain hospitals, provider specialties, long-term and post-acute care, behavioral health, etc.?
Are there specific use cases for data integration that your organization has focused on? If yes, what are they and how did you select them?
Did your organization have to create or change any of your policies as part of your work to integrate outside data? If yes, how so?
Possible probes:
a. Does your organization have any policies governing data provenance?
b. Are there privacy and security policies you had to navigate to integrate outside data?
How has your organization funded your data integration efforts?
Possible probes:
a. Are they grant funded, or infrastructure funding from payers or incentive payments?
b. Do you have a sustainable funding source to maintain them?
Environmental Factors
The next set of questions are about environmental factors in the market you serve, as well as aspects of the policy environment affecting data integration.
Are there characteristics of the health care market you are in that facilitate or impede data integration?
How would you describe the level of competition among health care providers in your market? How does this affect data sharing and integration?
Are there dominant EHR vendors in the market? How does that affect data sharing and integration?
Possible probes:
Are there any vendor practices that affect data sharing and integration (such as information-blocking?)
What role does the state or regional Health Information Organization (HIO) play in data integration in your market?
Possible probes:
Is there widespread participation in the HIO? Are they a key driver of interoperability in your market, or is some other mode of exchange?
What role do various payers (Medicare, Medicaid, private insurers) play in data integration?
Possible probes:
Is the Accountable Care Organization (ACO) penetration in your market a factor affecting data integration?
Are there state or federal policies that have affected the whether and how data integration is occurring?
Possible probes:
What policies have been key drivers of data sharing and integration in your market?
b. Are there policies that have acted as barriers?
Are there policy changes that are needed to better promote more common and advanced data integration?
Looking ahead, are there certain policy or technological changes that you think will affect the way that data integration looks today?
Possible probes:
Will consumer-mediated exchange affect data integration? If yes, how?
How about increasing use of Application Programming Interfaces?
Will the Trusted Exchange Framework and Common Agreement (TEFCA) or US Core Data for Interoperability (USCDI) data standards affect data integration? If yes, how?
Outcomes of Data Integration
Our final questions are about the outcomes of your data integration efforts.
To what extent are the integrated data being used in the way that was intended for your organization?
Possible probes:
If not as much as intended, what are the barriers to their use?
Are there certain types of users that use the data more than others?
Are there certain types of data being used more than others?
Are the goals of your organization’s data integration efforts being achieved? Why or why not?
Possible probes:
How do you know? Are you collecting data on any outcomes?
What have you heard about the usefulness of the data from end users?
Are you seeing a return on investment?
Has data integration helped you achieve the goals of value-based care?
Is there anything else related to data integration and how it supports the delivery of value-based care that we haven’t discussed today that you think we should know?
According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless it displays a valid OMB control number. The valid OMB control number for this information collection is 0990-0421. The time required to complete this information collection is estimated to average 1 hour per response, including the time to review instructions, search existing data resources, gather the data needed, and complete and review the information collection. If you have comments concerning the accuracy of the time estimate(s) or suggestions for improving this form, please write to: U.S. Department of Health & Human Services, OS/OCIO/PRA, 200 Independence Ave., S.W., Suite 336-E, Washington D.C. 20201, Attention: PRA Reports Clearance Officer.
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| Author | Ramos, Christal |
| File Modified | 0000-00-00 |
| File Created | 2021-01-13 |
© 2026 OMB.report | Privacy Policy