Focus Groups on Oncology Indications
Focus Groups About Drug Products As Used by The Food and Drug Administration
Terminology Moderator Guide
Focus Groups on Oncology Indications
OMB: 0910-0677
Oncology Indications
Clinical Endpoints Terminology Focus Group Moderator Guide
A. WELCOME AND GROUND RULES
Thank you for taking the time to join us today. I am _______ from RTI, a non-profit research organization. This focus group is being sponsored by the Food and Drug Administration, or FDA. Our discussion will last about one hour. The purpose of this focus group is to ask you some questions about ads for drugs used to treat different types of cancer and get your thoughts about the ways that cancer treatments are talked about. [FOR POST-TREATMENT GROUPS] You all identified yourselves as having completed treatment for cancer, that is what you all have in common.
Before we start, I want to review a few important things.
Your participation today is voluntary and you have the right to stop being in the focus group at any time.
None of my questions are very personal, but you can choose not to answer any of them if you are uncomfortable. Just let me know that you prefer not to answer.
[FOR POST-TREATMENT GROUPS] You may choose to share information about your medical treatment or condition, but you don’t have to. Either way, I want everyone to be comfortable sharing. We will all aim to be as supportive as possible of each other during this group.
We are audio recording this discussion so that I can give you my full attention and not have to take notes. When writing up a summary of the focus groups, we will not include any information that could identify you. Your name, address, and phone number will not be given to anyone, and no one will contact you about this research after this group is over.
I have colleagues listening to our discussion and taking notes behind the glass. At the end of our conversation, I may go into the back to see if there are any last-minute questions for you.
We are also live-streaming our session so that other members of the research team who couldn’t be here today can observe our discussion remotely.
Anyone can speak, and I’d like to hear from everyone; you don’t need to wait for me to call on you, just make sure you speak up and speak one at a time.
Please set your cell phones to vibrate or turn them completely off. If you need to use the restroom, please feel free to step out and join us once you are done.
I am not selling anything, I do not work for the people sponsoring this research, and I haven’t created any of the things we’ll look at, so don’t hold back on giving me your honest opinions.
If you disagree with anything that is said, I want to hear about it. If something is confusing, please let me know. Even if you are the only person in the room who feels that way—your opinion represents hundreds of people who are not in this room today.
Most importantly, there are no right or wrong answers. None of these are trick questions. I want to know your opinions and about your experiences.
I am not an expert about the topics we are going to discuss today or a medical doctor, so you may have questions that I can’t answer. However, we do want to know about questions you have on the materials I’m presenting today. At the end of our discussion, I can give you a website address that may give you more information about some of the topics we’ve discussed.
Do you have any questions before we continue?
B. PARTICIPANT INTRODUCTIONS – WARM-UP
To start, I’d like to go around the room and introduce ourselves. When we get to you, please tell us:
Your first name and
One thing you like to do in your free time
C. TERMINOLOGY
I’d like to get your feedback on some medical terms you may or may not have heard before. Some of these terms relate to different diseases and conditions, but today we will be talking about these terms only as they relate to cancer, not any other diseases.
OVERALL SURVIVAL
The first one is “overall survival”. We’ll talk about it in a minute, but first, I’d like you to answer the 2 questions on page 1 of your workbook.
Have you heard the term “overall survival”? [MODERATOR PUT TERM ON FLIP CHART]
W
 here
have you heard this before? [PROBE:
TV ads, HCPs, caregivers]
[MODERATOR
WRITE ANSWERS ON FLIP CHART]
here
have you heard this before? [PROBE:
TV ads, HCPs, caregivers]
[MODERATOR
WRITE ANSWERS ON FLIP CHART]
What does this term mean to you? Who would like to share what they wrote in their workbook? [MODERATOR WRITE ANSWERS ON FLIP CHART]
[FOR POST-TREATMENT GROUPS] Did your doctor ever mention this term when discussing your cancer with you? If so, did they explain it? How did they explain it to you? What words did they use?
Here is a definition of overall survival. [MODERATOR SHOW DEFINITION ON FLIP CHART: The length of time that patients are still alive after starting treatment.] In the workbook, please turn to page 2 and answer the question.
W
 hat
are your first thoughts about this definition?
hat
are your first thoughts about this definition?
What do you find confusing about this definition?
What information would help you decide whether to try a drug that can help improve overall survival?
Imagine that you had to explain the idea of overall survival to someone who may not understand or have heard of the term. How would you explain it?
[FOR POST-TREATMENT GROUPS] Did your doctor explain this idea in a different way? How did they explain it to you? What words did they use?
PROGRESSION-FREE SURVIVAL
Next, we are going to talk about the term “progression-free survival”. Please answer the questions on page 3 of your workbook and then we’ll discuss.
Have you heard the term “progression-free survival”? [MODERATOR PUT TERM ON FLIP CHART]
Where have you heard this before? [PROBE: TV ads, HCPs, caregivers] [MODERATOR WRITE ANSWERS ON FLIP CHART]
What does this term mean to you? Who would like to share what they wrote in their workbook? [MODERATOR WRITE ANSWERS ON FLIP CHART]
[FOR POST-TREATMENT GROUPS] Did your doctor ever mention this term when discussing your cancer with you? If so, did they explain it? How did they explain it to you? What words did they use?
Here is a definition of progression-free survival. [MODERATOR SHOW DEFINITION ON FLIP CHART: The length of time after starting treatment that a patient lives with the disease but it does not get worse.] In your workbook, please turn to page 4 and answer the question, then we’ll discuss.
What are your first thoughts about this definition?
What do you think when you hear “gets worse”? What does that mean to you?
What do you find confusing about this definition? What did you find clear? Specifically, what were you thinking about? [PROBE on whether they thought about symptoms]
If the definition was a little different and said “the length of time after starting treatment that a patient lives with the disease but it does not grow or spread further” what would that mean? The same meaning or different?
What do you think are the benefits or good parts of using a drug that improves progression-free survival?
What information would help you decide whether to try a drug that can help improve progression-free survival?
So, if a drug increases progression free survival that might mean that it could increase how long a patient lives, but there is no information available to say whether the drug will actually help them live longer. [MODERATOR SHOW CLARIFYING TEXT ON FLIP CHART]
Imagine that you had to explain the idea of progression-free survival to someone who may not understand or have heard of the term. How would you explain it?
[FOR POST-TREATMENT GROUPS] Did your doctor explain this idea in a different way? How did they explain it to you? What words did they use?
OBJECTIVE RESPONSE RATE
Next, we are going to talk about the term “objective response rate”. Go ahead and answer the questions on page 5 of your workbook and then we’ll discuss.
Have you heard the term “objective response rate”? [MODERATOR PUT TERM ON FLIP CHART]
Where have you heard this before? [PROBE: TV ads, HCPs, caregivers] [MODERATOR WRITE ANSWERS ON FLIP CHART]
What does this term mean to you? Who would like to share what they wrote in their workbook? [MODERATOR WRITE ANSWERS ON FLIP CHART]
[FOR POST-TREATMENT GROUPS] Did your doctor ever mention this term? If so, did they explain it? How did they explain it to you? What words did they use?
Here is a definition of objective response rate. [MODERATOR SHOW DEFINITION ON FLIP CHART]: The proportion of patients whose tumor shrinks or who have a decrease in the number of detectable cancer cells in their body. In your workbook, please turn to page 6 and answer the question, then we’ll discuss.
What are your first thoughts about this definition?
What do you find confusing about this definition?
What information would help you decide whether to try a drug that can help improve objective response rate?
So, if a drug increases objective response rate that might mean that it could increase how long a patient lives, but there is no information available to say whether the drug will actually help them live longer. [MODERATOR SHOW CLARIFYING TEXT ON FLIP CHART]
Imagine that you had to explain the idea of objective response rate to someone who may not understand or have heard of the term. How would you explain it?
[FOR POST-TREATMENT GROUPS] Did your doctor explain this idea in a different way? How did they explain it to you? What words did they use?
D. COMPREHENSION EXERCISE
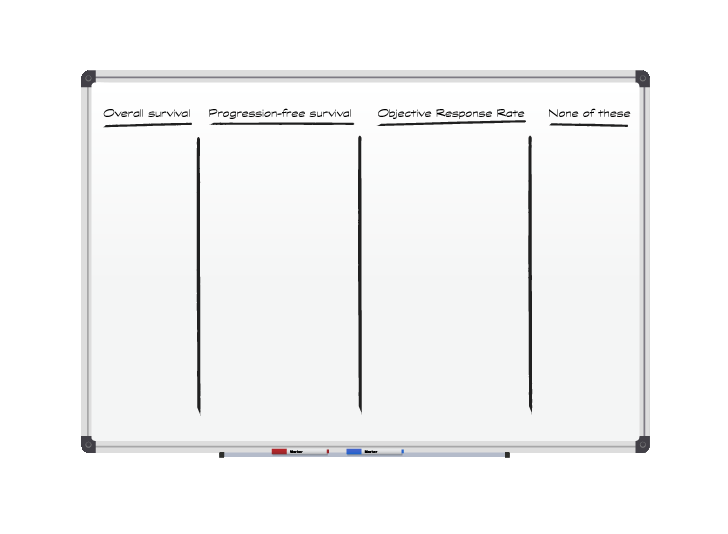
Next, I’d like to give you some examples and ask you to match them with one of the 3 terms we’ve talked about. We’ve removed the drug names, but these are all examples from prescription drug advertisements or websites. As a review, the 3 terms we have discussed are “objective response rate”, “progression-free survival” and “overall survival”. I’m also going to add in a “none of the above” option.
[MODERATOR WILL MAKE 4 COLUMNS ON WHITEBOARD FOR TERMS, READ EXAMPLES, THEN ASK GROUP TO MATCH THEM AND DISCUSS WHY. EACH OF THE CLAIMS BELOW WILL BE PRINTED ON NOTECARDS AND WILL BE STUCK UNDER THE COLUMN, OR COLUMNS, THAT PARTICIPANTS THINK THE CLAIM BEST FITS UNDER]
“In a clinical study, DRUG X, offered patients a longer life than chemotherapy.” [OS]
“At 5 years, more people taking DRUG X were living with their disease under control.” [PFS]
“Over 9 out of 10 (92%) people achieved some level of remission or response to therapy.” [OORR]
“DRUG X doubled the amount of time patients lived without their tumor spreading or growing.” [PFS]
Patients treated with DRUG X were 84% less likely to have their disease worsen or die during the trial compared to another approved therapy. [PFS]
In a clinical trial, 55.4% of women on DRUG X plus an aromatase inhibitor (AI) saw their tumors shrink versus 40.2% on an AI alone. [OORR]
DRUG X has been proven to help some patients live longer without their multiple myeloma getting worse. [PFS]
3.4% of women on DRUG X + an AI had a complete response, or no detectable sign of cancer, vs 0% with an AI alone. [OORR]
[PROBE AS NEEDED]
Is there anything more you want to know when you see these claims?
Would reading this information make you more or less likely to decide to use this drug? How so?
[FALSE CLOSE—TIME PERMITTING] We are almost done. I’m going to check with my colleagues to see if they have any other questions. [MODERATOR CHECKS FOR EXTRA QUESTIONS]
I want to thank each of you for coming and for participating today. These conversations will help us understand what information people need to make important health and treatment decisions for themselves and their family. We are looking to see how we can present this information so that it’s clear and people can feel confident and informed in their decisions. I mentioned earlier that I would give you a website if you want more information about some of the terms we talked about: www.cancer.gov [MODERATOR WRITE ON FLIP CHART] or talk to your healthcare provider.
OMB Control #0910-0677 Expires 05/31/2020
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| File Modified | 0000-00-00 |
| File Created | 0000-00-00 |
© 2026 OMB.report | Privacy Policy